TREATMENT/MANAGEMENT
Treatment begins with psychosexual education and counseling, in which underlying causes are addressed. The clinician educates the patient about the prevalence and common causes of painful intercourse, assessing what the patient has already done to alleviate the pain and reinforcing constructive and positive behaviors. It is therapeutic to validate the patient’s experience of pain and to explain that both pain and sexuality are mind and body processes. Even if the pain is due to a physical cause, it can have psychologic aspects or sequelae. The clinician normalizes the fact that pain associated with sex can cause anxiety and fear about participating in intercourse and that these are natural, instinctive reactions to pain.47
The patient is given an explanation of any physical and psychologic findings that might be contributing to her pain. This approach gives the patient hope for improvement with education and treatment. The emphasis is on the aspects of her sexual functioning that are still intact and positive features in her sexual history or relationship. A central goal is to minimize self-blame, hopelessness, and anxiety.
The patient is counseled about the need for adequate foreplay and stimulation to promote arousal and lubrication. Masturbation (alone and/or in conjunction with partnered sex) can be discussed as a way to increase vaginal lubrication, blood flow, and comfort with genital touch.
Another helpful strategy is to give the patient permission to take a hiatus from sexual intercourse.47 Women experiencing genital pain often avoid nonsexual affection and other sexual activities with their partners, fearing that they will lead to painful intercourse. In such cases, the woman is encouraged to form an explicit agreement with her partner that they will not have intercourse until she has made progress at managing her pain. The goal is to create greater openness to nonsexual affection and nonpenetrative sexual activity.
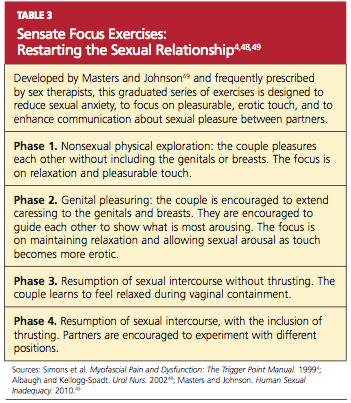
The clinician may suggest sensate focus exercises48,49 (see Table 3,4,48,49). In cases of vaginal atrophy and/or dryness, vaginal moisturizers and lubricants can help. Products containing perfumes, warming or tingling agents, parabens, and other chemicals can be irritating in some women.18
For the premenopausal patient using a low-dose oral contraceptive, the clinician’s instinct may be to provide a higher-dose estrogen pill. This may actually be counterproductive, however, because oral estrogen promotes synthesis in the liver of sex hormone–binding globulin, which then reduces circulating estrogen and can exacerbate the problem.50 Although the vast majority of women who use estrogen-containing oral contraceptives do not appear to develop symptomatic vulvovaginal atrophy, women who do experience bothersome atrophic symptoms may benefit from switching to an alternative contraceptive method (eg, an intrauterine device). Menopausal women may benefit from a topical estrogen product in the form of a vaginal ring, cream, or tablet.18,51,52
For vulvodynia, medical therapies such as topical anesthetics and centrally acting medications are under investigation. For cases of provoked vestibulodynia that do not respond to first-line treatment, patients may benefit from pelvic floor physical therapy, cognitive behavioral therapy aimed at pain reduction combined with sex therapy, or vestibulectomy.53,54
Addressing Bowel and Bladder Concerns
The patient with chronic constipation must be educated about the importance of adequate hydration and nutrition for bowel regularity. She is counseled about avoidance of straining or prolonged sitting during defecation and is offered primary treatment for hemorrhoids. A history of rectal bleeding, particularly in the absence of hemorrhoids, may be indicative of an anorectal or a colon malignancy, and the patient with such a history should be referred for further evaluation. The International Foundation for Functional Gastric Disorders (see “Resources” box) provides useful information for patients regarding constipation and associated pelvic floor disorders.
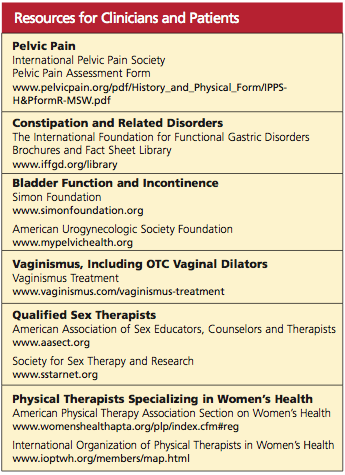
Urinary voiding prior to and following coitus or oral sex may reduce bladder discomfort and infection. Use of a dental dam for oral sex and good oral hygiene with regular dental care may also reduce the incidence of irritation and infection. Educational resources to address bladder function and incontinence can be found in the “Resources” box.
Treatment for Vaginismus
Vaginismus can be treated with desensitization techniques, including relaxation training, dilator therapy, pelvic floor therapy, and cognitive behavioral sex therapy, which teaches the patient to relax the introital muscles and give her the experience of controlled, pain-free penetration.55,56 A fundamental technique of relaxation training is deep breathing. Understanding the mechanics of breathing is important for physiologic quieting of the autonomic nervous system and facilitating relaxation of the pelvic floor.57
Dilator therapy can be used for treatment of vaginismus and vaginal stenosis, although in the presence of adhesions or a septum, lysis may be required first. A vaginal dilator can be inserted for approximately 15 minutes daily. Once the dilator passes easily with no painful stretching sensation, the patient should move to the next size larger dilator. The dilator can also be moved slowly and gently in and out and from side to side.
