The patient should be asked what she identifies as the source of her pain. What treatments have been tried, whether they have been helpful, and what treatments the patient thinks might be effective should all be addressed. The International Pelvic Pain Society34 offers a comprehensive pelvic pain assessment form (see box, “Resources for Clinicians and Patients,” below), which includes the short-form McGill Pain Questionnaire35 for describing and documenting characteristics of pain.
A detailed sexual function history begins with an assessment of sexual function in each domain (desire, arousal, orgasm).36 Other sexual problems, such as vaginal dryness, lack of desire or arousal, inability to experience orgasm, and forced or coerced sex should be identified. The clinician ascertains distress related to the patient’s sexual symptoms (eg, “How bothered are you by the pain you experience with intercourse?”). Information about her partner’s sexual functioning can be relevant, since delayed ejaculation may involve prolonged, ultimately painful intercourse.37 Commonly used objective assessment instruments for female sexual function include the Female Sexual Function Index (FSFI),38 the Sexual Function Questionnaire,39 and the Female Sexual Distress Scale (FSDS).40
A complete evaluation includes relevant medical, surgical, obstetric, and social history, along with a review of systems (see Table 1,34,38-40).
Medication History
A thorough assessment identifies OTC and prescription medications, including contraceptive methods. Long-term use of oral combined contraceptives has been associated with vaginal atrophy and vulvodynia.12 Clarifying whether the patient is using condoms with nonoxynol 9 is important, since this spermicide can cause painful irritation in some women.19 An allergy or sensitivity to latex in condoms or to chemicals in some lubricants can also cause irritation.
Physical Examination
The vulva should be inspected for signs of pallor, loss or thinning of hair, and clitoral shrinkage or shrinkage of the labia minora or majora. These can be signs of atrophy due to low estrogen. The vulva is also examined for skin changes, including inflammation, excoriation, scarring, fissuring, laceration, inability to retract the clitoral hood or complete loss of the clitoris by overlying tissue, and trauma.18 Additional assessment is needed for women with infundibulation in cases of female circumcision (also referred to as genital mutilation), as practiced in parts of the Middle East and Africa.30,41 A water-based lubricant, ideally warmed, can be used at the introitus and on the outer speculum blades to minimize discomfort during the exam without interfering with cytology, if a Pap smear is also being performed.42
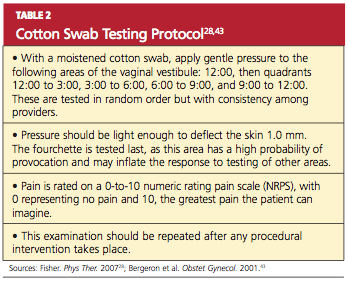
For women with introital pain, a “cotton swab test” is performed to quantify, localize, and map the pain (see Table 2,28,43).
The hymen is inspected and its morphology documented, particularly in the woman or girl with recent coitarche. The vagina is inspected for presence of a septum.14 Signs of atrophy include lack of lubrication, easy bleeding, fissures, discomfort even with use of a small speculum, and petechiae.18 Atrophic mucosa will appear flat and pale, with no evidence of normal rugae. The tissue’s elasticity will have decreased.
If there is suspicion of pelvic organ prolapse, vaginitis, or sexually transmitted infection, further assessments are made. Using one intravaginal finger if two fingers are painful, the clinician systematically palpates the urethra, bladder, bilateral fornices, posterior fornix, cervix, adnexa, and uterus in an attempt to reproduce the pain experienced during intercourse.29 Uterine size, contour, mobility, and any nodularity or irregularity are all noted.
During the pelvic examination, the clinician uses a hand mirror to show the patient the depth of penetration with the examining finger, a speculum, or a vaginal dilator—demonstrating the diameter of the introitus and vaginal canal, if possible. This is a valuable opportunity to educate the patient regarding her genital anatomy in addition to any physical findings that might explain her pain.
A rectovaginal examination is important for identifying constipation, hemorrhoids, or nodules along the rectovaginal septum or uterosacral ligaments, possibly indicating endometriosis.21,22 In patients with anal fissures, tensing of the anal sphincter and pelvic floor muscles to slow defecation (or to restrict the diameter of the feces) can result in a paradoxical contraction of the puborectalis portion of the levator ani muscles.28 This creates a vicious cycle of pelvic floor muscle spasm.
Pelvic floor function and strength are systematically evaluated using the Modified Oxford Scale44 or the Brink Scoring System.45 Scoliosis and hip height are assessed by asking the patient to bend over and touch her toes. Curvature of the spine or unequal hip height may indicate musculoskeletal problems that can cause or contribute to pelvic pain during intercourse.
Laboratory Workup
The vaginal maturation index18,46 may be assessed by taking a specimen for wet prep in the office setting or by sending a fixed smear on a slide or in a liquid cytologic preparation to a cytopathology laboratory. Vaginal pH, in combination with a wet prep, can be obtained to help assess for bacterial vaginosis or vaginal candidiasis. Laboratory tests are not regularly required, however, to diagnose and treat dyspareunia. Nevertheless, dyspareunia of musculoskeletal origin may require diagnostic neuromuscular evaluation, including EMG, ultrasonography, and manual assessment.28 These are commonly performed by a physical therapist with expertise in pelvic physical therapy and women’s health.