After we transitioned to a new vendor-based EHR in 2015, we developed a new medication reconciliation metric, aimed to align with Stage 2 MU requirements, and ensured all divisions had processes in place to review and reconcile medications. In our new EHR, medications lists are shared and viewable between ambulatory and inpatient environments and discharge summaries contain changes made to medications while inpatient. We have found that our performance on our new metric is 70.5% for February 2017 and we are continuing to educate physicians and staff on our new EHR functionality, our new electronic measurement and on workflows to help assist with improving performance with a short-term goal of 80%. We have found that our new EHR functionality does not match the ease of our old EHR functionality, which has made improvement on this metric a significant challenge for our clinicians and staff.
Maintenance of Certification
As of 2013, physicians who were board certified by the ABIM or ABMS were required to attain 20 practice assessment points showing participation in quality improvement activities for maintenance of certification (MOC). Although ABIM suspended the practice assessment requirement in 2015, it is likely that some component of quality improvement will be assessed in the future [5,19]. Prior to the changes in 2015, we were approached by the hospital leadership to roll out a new, streamlined process to leverage our existing quality metrics and established performance improvement plans in order to allow physicians to gain MOC credit. Each metric/project was vetted with 3 separate groups: the DOMQP, hospital leadership leading the MOC efforts, and Partners Healthcare, our overarching local health care system. We worked with our division physician champions and the physicians preparing for board re-certification to complete the one-time documentation required by the hospital for MOC. This process took approximately 6 months per project. Once the project was approved by all 3 channels, all physicians participating in the quality effort could get the practice assessment points by completing a simple attestation form.
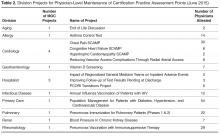
For example, the DOMQP had already developed a metric with our allergy division measuring use of the Asthma Control Test during office-based visits. During one of our faculty meeting presentations, we shared that Partners now had a pilot program to count current QI projects at the hospital for MOC points. We asked for interested volunteers and worked with 1 or 2 physicians who most often were up for recertification that year. DOMQP provided the data that we already managed and prepopulated the required application and PowerPoint. The physician adds text regarding the clinical relevance of the project, how the improvement strategies in clinic evolved over time, and barriers faced in achieving their goal. The DOMQP sends the documents to Partners for review, and once the project is accepted, the division chief forwards attestation forms to participating physicians. To be eligible, a physician had to have data present in our monthly reports with at least 10 patients in their denominator. Some division chiefs included the additional criterion that a provider also had to be at goal performance set by the division in order to attest and receive MOC points. To date we have 15 projects approved with 206 physician attestations submitted for MOC points (Table 2) . Through the aid of the Partners Healthcare Office of Continuing Professional Development we are now able to offer physicians assistants AMA PRA Category 1 credit for participation in division projects. Having an easy process that builds on existing DOMQP efforts has been a highly valued resource to our faculty. As the MOC process was de-emphasized by ABIM, we have shifted our focus to the changes surrounding the Quality Payment Program and are aligning our project-based work to support quality measurement and improvement.