In 2010, the VHA implemented the patient-centered medical home model of primary care health care as part of its transformational T-21 Initiatives.1 Now known as Patient Aligned Care Teams (PACTs), the key pillars of the model include the expanded roles and responsibilities of multidisciplinary care teams who provide enhanced access and coordinated care. This model is based on a foundation of adequate resources, patient centeredness, and process improvement (Figure 1).
The national implementation strategy consisted of an initial educational conference with 3,600 attendees. The conference included a series of PACT learning collaboratives that engaged > 300 primary care teams, 5 demonstration laboratories, and educational outreach through learning centers and on-site consultations. Despite an aggressive national implementation plan, many frontline primary care teams struggled to translate the medical home theory into process.
Background
The Richard L. Roudebush VAMC (RLRVAMC) is a large tertiary medical center providing care to > 44,000 primary care patients. This care is delivered by 58 primary care physicians (PCPs) in 5 hospital-based outpatient clinics, including 1 large teaching clinic, 3 community-based outpatient clinics (CBOCs), and a clinic that serves recently returned active-duty veterans. Administrative nursing and clerical associates report to the Office of Ambulatory Care, and physicians and nurse practitioners report to the Medicine Service. Before the implementation of the PACT model, the functional unit of primary care was an entire clinic, typically consisting of 4 to 10 PCPs, nurses, and clerical associates.
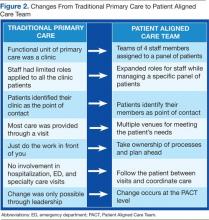
Discussions about process change had previously occurred through monthly service or clinic meetings in which administrative leaders provided direction to frontline staff. This culture of top-down leadership drove process change but was not always effective and empowering for practice change. With the implementation of PACT, the functional unit of primary care shifted from the larger clinic to a team composed of a PCP, a nurse, a licensed nurse practitioner or health technician, and a clerical associate.
The care delivery system fundamentally changed from the traditional model to a medical home model (Figure 2). This group now represented the fundamental clinical microsystem for the delivery of primary care within the VA medical home model.2 The experience of Batalden and colleagues at the Dartmouth Hitchcock Medical Center suggests that such microsystems are very effective units of change.3 The key challenge presented to the primary care leadership was how to link these clinical PACT microsystems with an effective process that would guide practice redesign.
The concept of practice coaching or facilitation as a mechanism for physician offices to adopt evidence-based medicine and quality improvement dates to the early 1980s in England. This model spread to the U.S. in the 1990s and has continued to be used as a mechanism for leading clinical practice redesign.4 In traditional practice facilitation, a trained individual is brought in from outside the practice to help adopt evidence-based medicine guidelines.5 This individual works with the practice to implement changes that translate into patient outcome improvements.
Unlike consultation, this facilitator maintains a long-term relationship with the team as they work together to achieve goals. More important, the facilitator assists the team in developing improvement processes that are sustainable as they become incorporated within the fabric of the team culture and remain after the coach is gone. There are several reviews of clinical practice coaching that support its effectiveness in implementing evidence-based primary care guidelines.6,7 The Affordable Care Act contains provisions for the use of this model in promoting best practices and quality care.8 Manuals developed by the Agency for Healthcare Research and Quality outline how to develop a practice facilitation program.9,10
Related: Infusing Gerontologic Practice Into PACT
Essential to all practice facilitation models is the effective use of quality improvement tools. The RLRVAMC adopted the VHA Lean Healthcare Improvement Framework, which includes an approach for rapid cycle change.
The RLRVAMC adopted the facilitative coaching model in November 2011, using internal coaches who were assigned to the fundamental microsystem of its medical home.
Coach Selection
Many facilitative coaching models described in the literature use external coaches. Frequently cited advantages of external coaches include having dedicated time, receiving standardized training in facilitation, and being regarded as neutral to internal conflicts. The RLRVAMC staff elected to identify internal coaches. Advantages of this approach include the use of existing resources, the ability to develop long-term continuous relationships with PACTs, and the ability to access key internal resources to assist the team. Also, using internal individuals holding primary care leadership positions was critical to the coaching model.
Thirty-eight PACTs were initially created, and 15 internal coaches were identified. These individuals included the associate chief of staff of Ambulatory Care, chief nurse for Clinic Operations, business administrators in primary care, and all frontline unit managers and supervisors. This level of management involvement provided content expertise about primary care operations and equally important, carried the authority to implement change.