CASE
A 28-year-old active woman presented to our clinic 22 months after sustaining a right knee tibial eminence fracture that was initially treated with extension immobilization, which resulted in a fibrous malunion. She subsequently sustained a second injury resulting in displacement of the malunion fracture fragment, and was treated at another institution 10 months prior to presentation at our clinic with arthroscopic reduction and internal fixation with a cannulated screw and washer of the tibial eminence fracture. This was followed by hardware removal 6 months prior to her office visit at our clinic. At presentation, she reported worsening right knee pain, mechanical symptoms, and loss of both flexion and extension compared with her uninjured knee. Conservative management, including activity modification, extensive physical therapy, and anti-inflammatory medication following her most recent procedure, had not resulted in improvement of her symptoms.
Physical examination revealed significantly reduced knee flexion and extension (+15°-120° on the affected side compared with 5° of hyperextension to 130° flexion of the contralateral knee). Ligamentous examination demonstrated no laxity with varus or valgus stress at 0° to 30° of flexion, negative posterior drawer, and a Grade 2 Lachman and positive pivot shift. She also exhibited pain with attempted right knee terminal extension. Radiographs and computed tomography scans were obtained and reviewed. They revealed a malunited tibial eminence fracture (Figures 1A-1D).
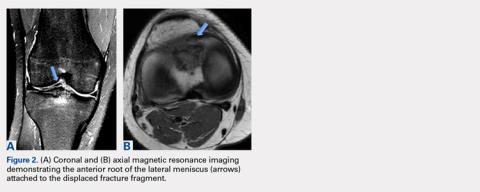
The fragment was located anterior and lateral to its native location, which created a mechanical block during knee motion. Additionally, MRI demonstrated that the anterior horn of the lateral meniscus was displaced and attached to the malunited fragment (Figures 2A, 2B) as well as to nonfunctional ACL fibers. On the basis of the mechanical block restricting extension and the displaced anterior horn of the lateral meniscus compromising meniscal function, we recommended arthroscopic surgery. After discussion of the risks and benefits of the procedure with the patient, she provided informed consent, and it was decided that the patient would undergo arthroscopic fragment excision followed by anatomic repair of the anterior root of the lateral meniscus, and that we would proceed with ACL reconstruction in the future given her subjective instability and physical examination findings of ACL insufficiency.Arthroscopic assessment of the right knee demonstrated the large osseous fragment located in the anterolateral aspect of the joint with the displaced anterior horn of the lateral meniscus attached as well as significant anterior impingement limiting knee extension. Probing of the anterolateral meniscal root in the lateral compartment showed abundant surrounding scar tissue with an abnormal attachment, representing a chronic root avulsion. A mechanical shaver was used to débride the scar tissue and expose the malunited fragment, followed by complete osseous fragment excision with a high-speed burr (Figure 3).
The knee was taken through full range of motion (ROM) from 5° of hyperextension to 130° of flexion with arthroscopic confirmation of no further anterior impingement.A soft tissue anterolateral meniscal root repair was performed by creating a 2-cm to 3-cm incision on the anterolateral tibia, just distal to the medial aspect of the Gerdy tubercle. To best restore the footprint of the repair and increase the potential for biologic healing, 2 transtibial tunnels were created at the location of the root attachment. An ACL aiming device with a cannulated sleeve was used to drill 2 bony tunnels approximately 5 mm apart, exiting at the anatomic root footprint. The drill pins were removed, leaving the 2 cannulas in place for later suture passage. A suture-passing device was used to pass 2 separate sutures through the detached meniscal root.
A looped passing wire was directed up the previously placed cannulas, and 1 suture was shuttled down each tunnel. The sutures were securely tied down over a bony bridge with a cortical fixation button on the anterolateral tibia. This was visualized arthroscopically to ensure proper positioning and tension of the root to its native footprint (Figure 4). A comparison of preoperative and postoperative anteroposterior and lateral knee radiographs is shown in Figures 5A, 5B.Continue to: Postoperatively, the patient was placed...