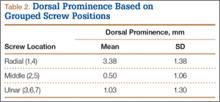
Mean (SD) dorsal prominence at each screw position was calculated. The screws were also categorized into radial (1,4), central (2,5), and ulnar (3,6,7) groups based on location within the plate (Figure 3). Equality of means testing was performed using a 1-way analysis of variance followed by a Bonferroni test.
Results
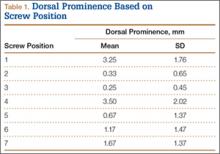
Mean (SD) dorsal prominence in millimeters is listed in Table 1. Positions 1 and 4 had significantly more dorsal prominence than the other 5 screw positions (P < .01 for all comparisons). Mean (SD) dorsal prominence based on grouped screw positions is listed in Table 2. There was significantly more dorsal prominence in the radial group that in the central group (P < .001) and ulnar group (P < .001). Mean depth of the Lister tubercle was 3.25 mm.
All prominent screws in the radial aspect of the radius were detected using a supinated 45° view. A 45° pronated view was not successful in demonstrating screw prominence on the ulnar side of the wrist because of overlap of the ulnar head.
Discussion
Extensor tendon irritation and extensor tendon rupture are frequent yet preventable complications of using volar plating systems to stabilize distal radius fractures. Many recent studies have investigated the intraoperative methodologies in order to identify real-time adjustments the surgeon can make to prevent negative outcomes. The first report of extensor tendon injury caused by volar plate fixation (published in 1989) was attributed to dorsal screw prominence.9,10 Even today, extensor tendon complications remain a challenge, as screw prominence is difficult to ascertain even with multiple intraoperative radiologic views.1,8
This study simulated real-time radiographic views to estimate if screws had extended into the dorsal compartment. These radiographic predictions were then correlated with the absolute dorsal screw prominence seen after dorsal compartment dissection. We determined that the supinated oblique view was the best imaging view for identifying radial styloid screw prominence.
Mean depth of the Lister tubercle was 3.25 mm (similar to previously reported 2 mm11). However, there was no correlation identified between depth of the Lister tubercle and amount of dorsal screw prominence.
We wanted to identify high-risk areas and estimate expected dorsal screw prominence in order to make appropriate intraoperative screw length adjustments. The radius is divided into radial, central, and ulnar columns. The central screw positions had the least dorsal screw prominence (mean, 0.50 mm). This central position was considered low-risk. Both the radial and the ulnar screw positions had more dorsal screw prominence (means, 3.38 mm and 1.03 mm, respectively). Only the radial screws had significantly more prominence. However, this study was not powered to detect a difference as small as that between the central and ulnar screw positions. Despite the lack of statistical significance, it is clear from the data that the ulnar screws trend toward more dorsal prominence, and, therefore, screw measurements at both the radial and ulnar screw locations (using the depth gauge) require adjustments.
Extensor tendon contact was difficult to determine based on any specific screw length, as the extensor tendon had to be dissected to determine prominence. Based on observations, a prominence of 2 mm seemed to present a risk for tendon irritation. The periosteum and the rounded end of the screw may obviate the risk with 1 mm of prominence. However, this observation may not hold true in an in vivo situation.
This study had several limitations. First, only a single brand of plate was used, making these findings specific to this system. However, concepts and conclusions can be extrapolated to all systems. The radial side had the highest risk for prominence, and this factor should be accounted for when selecting screw lengths. In addition, the ulnar column also poses some risk, but not to the degree of the radial column. Another limitation is that fractures were not created in these radii; therefore, dorsal comminution was not recreated. In some cases, the dorsal cortex may be displaced dorsally and be somewhat protective. This study is not meant to be an exhaustive study on all volar plates or provide absolute recommendations. It is meant to suggest caution to surgeons who may not be familiar with the complex anatomy of the dorsal radius and to identify areas where the risk for screw penetration is highest.
Shortening screw lengths at the positions described may trigger surgeons’ concerns about stabilizing distal radius fractures. In a 2012 biomechanical study, Wall and colleagues12 found no difference between unicortical screws (placed at 75% of the distance to the dorsal cortex) and bicortical screws in effectiveness in stabilizing distal radius fractures.12 The proposed reduction will result in the desired bicortical screw lengths but limit prominence. In addition, in the setting of dorsal comminution, the increased stability gained by bicortical fixation is minimal.