Behavioral therapy. Specialized treatments developed specifically for teen smoking cessation—such as Not On Tobacco (see Related Resources)—often are delivered in schools or other group settings. The most successful consist of ≥5 sessions and include motivational enhancement, cognitive-behavioral, and social influence-oriented approaches.30
Other behavioral treatments. Most psychiatrists are not equipped to deliver these specialized behavioral treatments. Instead, you can use simple yet effective behavioral treatments during routine office visits as adjuncts to pharmacotherapy. At the very least, we recommend the U.S. Public Health Service’s “5 As” strategy (Box 2).16
Educate patients about what to expect during withdrawal, how long withdrawal will last, and medication side effects. To help adolescents develop appropriate treatment expectations:
- discuss the difference between a “slip” (having 1 cigarette) and a “relapse” (returning to daily smoking)
- explain that many individuals need multiple attempts before they quit.
Encourage adolescent smokers to contact the National Network of Tobacco Cessation Quitlines (1-800-784-8669; www.smokefree.gov), which provides free access to telephone-based counseling services.
Ask every patient about tobacco use during every visit, and have a system for recording and tracking tobacco use in the chart
Advise patients clearly and unambiguously to stop smoking, and tailor that advice to each patient’s needs
Assess every patient’s readiness to quit
Assist patients who are ready to quit through self-help materials, referral, and/or smoking cessation treatment
Arrange follow-up visits for relapse prevention or to reassess readiness to quit
Source: Reference 16
Choosing treatment
Evidence guiding treatment choice for teen smoking cessation is limited but growing. Most studies examined daily cigarette smoking, with significantly less evidence to support treatment decisions for light (non-daily) smokers and teens who use other tobacco products.
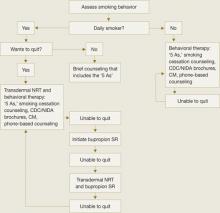
Recommendations.We have developed a strategy to guide treatment of adolescent smokers (Algorithm). We recommend using pharmacologic interventions only for teens who smoke daily because:
- most studies have focused on daily smoking
- efficacy data are limited
- pharmacologic interventions carry potential risks.
Because of bupropion SR’s contraindications and potential side effect profile, we suggest NRT in combination with smoking cessation counseling as a first-line treatment for young smokers. We recommend beginning with transdermal NRT because of the low likelihood of underdosing with the patch’s once-daily application.20 With either NRT or bupropion SR, schedule follow-up appointments to target relapse prevention and solve any issues that arise.
Help your patient choose a “quit date,” preferably 1 to 2 weeks after your initial assessment. We recommend encouraging young smokers to reduce their smoking by 1 cigarette per day to help minimize withdrawal symptoms from “cold turkey” cessation.31
Some physicians have found it helpful to see the patient on the quit day—or 2 days after when withdrawal symptoms tend to be most robust—to provide support and encouragement. Ask the adolescent to bring and discard during the visit all smoking paraphernalia as a symbol of his or her new smoke-free status.
Step 1: NRT. Initiate smoking cessation counseling plus transdermal NRT using the dosing guidelines in Table 3,28,31 and adjust the dose depending on severity of withdrawal symptoms. Ideally, the patch delivery will be used for 12 weeks, with at least 3 and ideally 6 weeks on the initial dose, followed by a gradual taper.28 We strongly recommend using transdermal NRT on adolescent inpatient units, especially for daily smokers and those who exhibit nicotine withdrawal symptoms.
Step 2: Bupropion SR. If NRT fails, the next step is bupropion SR plus smoking cessation counseling, assuming the adolescent does not have contraindications to bupropion SR. Start the medication based on the dosing guidelines in Table 3,28,31 and set a quit date for 2 weeks after starting bupropion SR.
Again, encourage adolescents to reduce by 1 cigarette per day over the 2 weeks before the quit day to minimize withdrawal symptoms.31 Continue bupropion SR for at least 8 and optimally 12 weeks.31
Combination therapy? If teens are unable to successfully quit smoking with NRT or bupropion SR alone, experience with adults suggests combining the 2 therapies might be beneficial. However, no evidence supports combination therapy in adolescents. Instead, consider referring adolescents who can’t quit to a smoking cessation specialist.
AlgorithmA strategy to initiate smoking cessation in adolescents
CDC: Centers for Disease Control and Prevention; CM: contingency management; NIDA: National Institute of Drug Abuse; NRT: nicotine replacement therapy
Source: Adapted from Upadhyaya H, Deas D, Brady K. A practical clinical approach to the treatment of nicotine dependence in adolescents. J Am Acad Child Adolesc Psychiatry 2005;44(9):942-6 with permission of Lippincott Williams & Wilkins.Table 3