Recovery without treatment is rare. The typically early age at onset of generalized SAD3,4 imposes greater limitations on development of social competence than on those who develop more discrete fear of public speaking or performing later in life—after socialization skills have already developed.
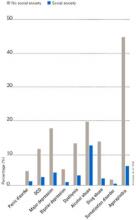
Individuals with SAD frequently suffer from comorbid psychiatric disorders, mostly depression and/or other anxiety disorders.6Figure 1 shows that individuals with SAD are at significantly increased risk for depression, other anxiety disorders, and alcohol and drug abuse. Since generalized SAD usually appears at an earlier age than other anxiety disorders, it represents a risk factor for subsequent depression. The level of functional impairment caused by SAD is similar to that caused by major depression7 (Figure 2).
As more comorbid psychiatric disorders accrue, impairment and increased risk for additional disorders may occur. Further, the risk of suicide is increased in those with comorbid SAD vs. those with SAD only. The findings suggest that if social anxiety were detected and treated effectively at an early age, it might be possible to prevent other psychiatric disorders—particularly depression—as well as the predictable morbidity and mortality that accompanies untreated SAD. Given the estimated $44 billion annual cost of anxiety disorders in the U.S.,8 research targeted at testing this hypothesis would appear to be a good investment.
Figure 1 HOW PREVALENT IS LIFETIME COMORBIDITY IN SAD?
- Inherent avoidance of scrutiny, (e.g., evaluation)
- Uncertain diagnostic threshold
- Acceptance of pathological shyness as ‘just my personality’
- Lack of understanding by professionals, family, friends
- Coping strategies that mask disability
- Comorbid psychiatric disorders that mask SAD
Figure 2 QUALITY OF LIFE IN PATIENTS WITH SOCIAL ANXIETY DISORDER
Seeing the unseen: making the diagnosis quickly
Although SAD is extremely common, a variety of factors may contribute to the low rate of recognition of the disorder (Box 3). Because of their intense discomfort toward scrutiny by authority figures such as their physician, individuals with SAD may not be willing to discuss their fears. Studies estimating the prevalence in primary care suggest that these individuals visit their referring physicians at about the same rate as the general population.6,9-11 Affected individuals are unlikely to seek psychiatric treatment unless they have a comorbid depression or anxiety.6,7
Table 1
DIFFERENTIAL DIAGNOSIS FOR SOCIAL ANXIETY DISORDER
| Condition | Diagnostic features |
|---|---|
| Posttraumatic stress disorder | Temporally follows traumatic event; cues related to trauma, not exclusively to social situations |
| Panic disorder | Unexpected panic attacks, not exclusively socially mediated anxiety |
| Agoraphobia | Fearful avoidance of situations in which panic attacks may occur, not limited to social situations |
| Major depression or atypical depression | Social withdrawal temporally related to mood disturbance, not to fear of humiliation or embarrassment; atypical depression with rejection sensitivity associated with other symptoms (e.g., hypersomnia, hyperphagia, anergy, mood reactivity) |
| Generalized anxiety disorder | Focus of worry not limited to social situations; social discomfort or avoidance not a key feature |
| Body dysmorphic disorder | Avoidance of social activity focused on concern over perceived ugliness |
| Avoidant personality disorder | Often present in generalized social anxiety disorder; may represent more severe end of social anxiety disorder spectrum; social activity desired but avoided |
| Schizotypal/schizoid personality disorders | Avoidance of social situations is preferred by individual and is not due to fear of embarrassment or humiliation |
| Normal shyness | Minimal or no interference with social, occupational, or family functioning |
| Adapted from Lydiard RB. Social anxiety disorder: comorbidity and its implications. J Clin Psychiatry.2001;62(suppl 1):17-23. | |
SAD can be difficult to tease apart from other coexisting conditions. Individuals who present for treatment of other anxiety disorders, depression, or substance abuse disorders should be considered at risk for current but undetected SAD. Many of the symptoms overlap (Table 1). The key diagnostic feature, which leads to the diagnosis of SAD, is that the fear and avoidance specifically are related to being in or anticipating a feared social situation (Box 4).
Social
- Attending parties, weddings etc.
- Conversing in a group
- Speaking on the telephone
- Interacting with authority figure (e.g., teacher or boss)
- Making eye contact
- Ordering in a restaurant
Performance
- Public speaking
- Eating in public
- Writing a check
- Using a public toilet
- Taking a test
- Trying on clothes in a store
- Speaking up at a meeting
Many clinicians mistake social anxiety for panic disorder, since panic attacks in people with SAD are often cued by social situations. There can be up to a 40% overlap of SAD with panic disorder.4 Without probing carefully into the focus on fear and avoidance, SAD can be easily overlooked. Individuals with panic disorder experience unexpected attacks and are terrified at the prospect of additional attacks, while those with SAD experience attacks linked to social situations and fear scrutiny and embarrassment more than the attacks themselves.