Although Ms. S appeared thin, her BMI was within normal range. She added that she likes food and enjoyed eating, but that her medical condition made it too painful. Lastly, Ms. S denied a history of binging or purging.
Somatic symptom disorder. Table 11 outlines the DSM-5 criteria for somatic symptom disorder. A diagnosis of somatic symptom disorder requires ≥1 somatic symptoms that cause enough distress to significantly disrupt daily functioning. Furthermore, the patient is characteristically preoccupied with excessive thoughts, feelings, or behaviors as they relate to the health concern, manifested by at least 1 of the following: disproportionate and constant thoughts about the seriousness of the somatic symptom; continuous high anxiety with regard to health or somatic symptoms; and excessive time and energy spent worrying about these somatic symptoms or “health concerns.”1,2
Factitious disorder imposed on self. An individual with FDIS chronically stimulates, induces, or aggravates illnesses to gain the status of being a patient.
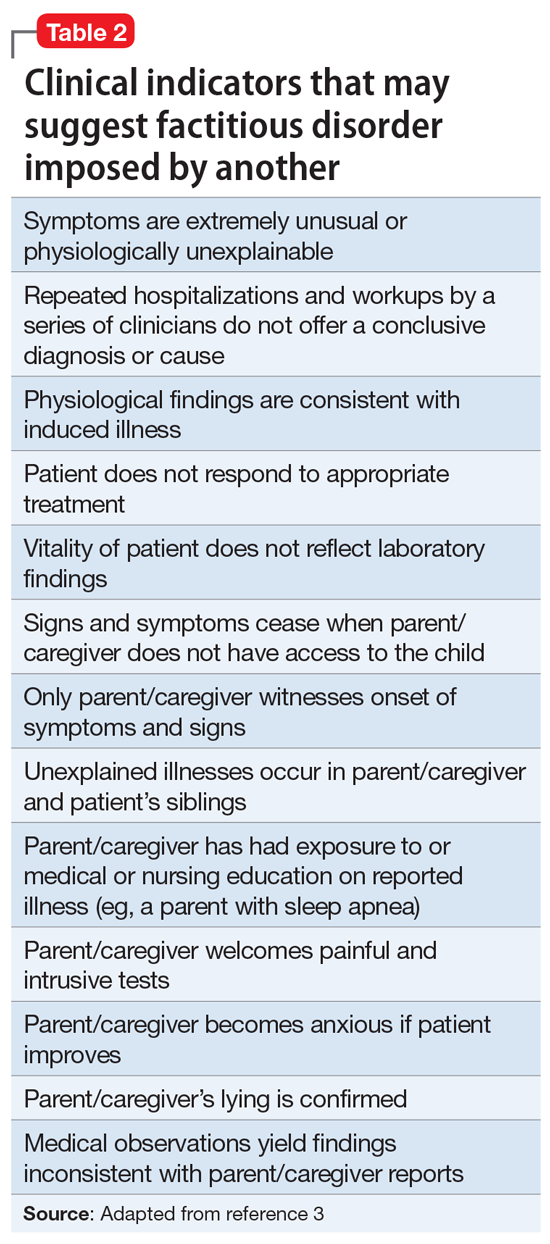
Factitious disorder imposed on another is the deliberate feigning or production of symptoms in another individual who is under the perpetrator’s supervision.1 Table 23 lists clinical indicators that raise suspicion for FDIA.
Before a diagnosis of somatic symptom disorder, FDIS, or FDIA could be established or ruled out, it was imperative to gather collateral information from other clinicians involved in Ms. S’s care. Ms. S and her mother had sought out help from a pediatric surgeon, a pediatric gastroenterologist, a pediatrician, and a psychotherapist.
Continue to: EVALUATION Collateral information