From the Editor
Let’s increase our use of IUDs and improve contraceptive effectiveness in this country
The unintended pregnancy rate is too high in the United States, and the use of long-acting reversible contraceptives is too low. Expanding the...
Melissa J. Chen, MD, MPH
Dr. Chen is a Family Planning Fellow in the Department of Obstetrics and Gynecology at the University of California, Davis, in Sacramento, California.
Mitchell D. Creinin, MD
Dr. Creinin is Professor and Chair of the Department of Obstetrics and Gynecology at the University of California, Davis, in Sacramento, California.
Dr. Chen reports no financial relationships relevant to this article. Dr. Creinin reports that he receives research funding from Medicines360 and is a consultant for Merck.

Details of the study
To evaluate real-life outcomes, Gariepy and colleagues performed a decision analysis to estimate the probability of pregnancy after hysteroscopic sterilization and laparoscopic approaches with silicone rubber band application and bipolar coagulation. Using a Markov state-transition model, the authors could determine the probability of pregnancy over a 10-year period for all types of sterilization. For hysteroscopic sterilization, each of the multiple steps, from coil placement to use of alternative contraception in the interim period to follow-up confirmation of tubal occlusion, could be included.
At 10 years, the expected cumulative pregnancy rates per 1,000 women were 96, 24, and 30 for hysteroscopic sterilization, laparoscopic silicone rubber band application, and laparoscopic bipolar coagulation, respectively. For hysteroscopic and laparoscopic sterilization to be equal in effectiveness, the success of laparoscopic sterilization would need to decrease to less than 90% from 99% and hysteroscopic coil placement or follow-up would need to improve.
The authors concluded that the effectiveness of sterilization does vary significantly bythe method used, and rankings of effectiveness should differentiate between hysteroscopic and laparoscopic sterilization.
What this evidence means for practice
When counseling women about sterilization, we should discuss the advantages and disadvantages of hysteroscopic versus laparoscopic approaches and disclose the efficacy rates of each method.
The issue is not that the hysteroscopic sterilization procedure is less effective than laparoscopic sterilization. The real take-home point is that women choosing to attempt hysteroscopic sterilization are more likely to experience an unintended pregnancy within the next 10 years than women presenting for laparoscopic sterilization.
Each year, 345,000 US women undergo interval sterilization.6 If hysteroscopic sterilization were attempted as the preferred method for all of these women (as compared with laparoscopic sterilization) in just 1 year, then an additional 22,770 pregnancies would occur for this group of women over the ensuing 10 years. With the current technology, hysteroscopic sterilization should be reserved for appropriate candidates, such as women who may face higher risks from laparoscopy.
WE WANT TO HEAR FROM YOU! Share your thoughts on this article. Send your Letter to the Editor to: rbarbieri@frontlinemedcom.com
The unintended pregnancy rate is too high in the United States, and the use of long-acting reversible contraceptives is too low. Expanding the...
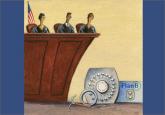
Contraception now is covered for most insured patients, but two cases before the Supreme Court could unravel this new guarantee
This overview of vessel-sealing devices for laparoscopic procedures should help you select a system that meets the particular needs of your...
When it comes to the morning-after pill, physicians need a wake-up call

Although it is gaining popularity in the United States, the IUD is often overlooked as a contraceptive option because of several common...
Unpredictable bleeding with progestin-only contraceptives can lead to dissatisfaction and discontinuation. The authors scrutinize the reported...
