Clinical Review

2014 Update on abnormal uterine bleeding
Randomized data shed light on AUB associated with fibroids, adenomyosis, and the use of progestins
Amy Garcia, MD, is Director, Center for Women’s Surgery and Garcia Institute for Hysteroscopic Training, Albuquerque, and Clinical Assistant Professor, Department of Obstetrics and Gynecology, University of New Mexico School of Medicine, Albuquerque. Dr. Garcia serves on the OBG Management Board of Editors.
Dr. Garcia reports that she receives grant or research support from Hologic, Inc. She is a consultant to Bayer, Boston Scientific, Channel Medsystems, Ethicon, Hologic, IOGYN, Karl Storz Endoscopy, Minerva Surgical, and Smith & Nephew. She is a speaker for Ethicon.

MINIMALLY INVASIVE THERAPY FOR GYNECOLOGIC SYMPTOMS
van der Voet LF, Vervoort AJ, Veersema S, Bij de Vatte AJ, Brolmann HAM, Huirne JAF. Minimally invasive therapy for gynaecological symptoms related to a niche in the caesarean scar: A systematic review. BJOG. 2014;121(2):145-156.
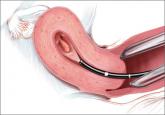
CSD-related bleeding issues may not respond to hormonal management and are frequently underdiagnosed. This scenario often leads to hysterectomy. Because there are women who desire uterine preservation, van der Voet and colleagues sought to evaluate the results of nonhysterectomy treatments of CSD-related AUB. They limited this systematic review to include only published studies that were randomized controlled trials, cohort studies, case-control studies, and case series of at least five patients.
Additionally, they included only studies that reported on conservative therapies (hysteroscopic resection, laparoscopic repair, abdominal repair, vaginal repair, endometrial ablation, LNG-IUS, or medical management) as well as at least one of the following outcomes: AUB, pain relief, sexual function, quality of life, surgical outcome, anatomic reconstruction, fertility or pregnancy outcome. Of 1,629 publications that were screened, 12 ultimately met inclusion criteria for the review. The studies, 11 of which were peer reviewed and 1 abstract, were published between 1996 and 2013 and reported on a total of 455 women with postcesarean AUB.
Weaknesses of the study
The most poignant statements made by the investigators pertain to the methodologic quality of the included articles. No study met requisite quality criteria. A clear definition of outcomes, including standardized measurements, was lacking in most studies. Most of the studies reviewed did not report CSD measurements, and only one study provided an objective reproducible method of CSD measurement. Few studies reported AUB symptom evaluation methodology, and no study used validated questionnaires. In the majority of studies, methods of posttreatment outcome measurements either were not reported or differed from pretreatment evaluation methods, potentiating verification bias. Because their literature review yielded primarily small case series publications that reported positive effects of interventions, and because of a lack of large RCT and prospective cohort trials, little could be gleaned regarding the viability of treatment interventions for CSD-related AUB.
Only three studies provided sufficient data to be included in a meta-analysis. The number of days of bleeding was reduced with hysteroscopic defect resection by 2 to 4 days in two studies, and in one study, vaginal repair decreased days of bleeding by 4 to 7 days. Only one study with laparoscopic repair compared CSD characteristics before and after surgery. Residual myometrial thickness increased for laparoscopic repair to greater than 8.3 mm; however, it is not known if this will make a clinical difference in the risk of scar dehiscence or improved functionality of the lower uterine segment.
Two studies reported on the laparoscopic repair of scar defects in asymptomatic patients, which is not recommended by these investigators. It is not known what ramifications hysteroscopic resection of the scar will have for the risk of uterine rupture, malplacentation or cervical incompetence for women who conceive after hysteroscopic repair.
Meaningful conclusions are lacking
Despite the high success rates reported by investigators of various surgical intervention case series involving hysteroscopic resection, vaginal repair, or laparoscopic repair, van der Voet and colleagues ultimately state that the methodologies of these studies do not allow meaningful conclusions to be drawn regarding the effectiveness of any of these interventions. Consequently, the authors recommend that the outcomes of their meta-analysis be scrutinized. They also point out that the LNG-IUS has proven benefit for AUB and yet has not been studied in the treatment of AUB associated with a CSD.

Randomized data shed light on AUB associated with fibroids, adenomyosis, and the use of progestins

How to assess technology and apply new findings to patient care
Understanding of abnormal uterine bleeding has been hampered by inconsistent use of terminology and a lack of classification of its causes, but...
