FIGURE 2 Laparoscopic port placement
Place the camera through the umbilical port (A) and operate through two additional ports on the left-hand side of the patient, where the primary surgeon stands. Place the first operative port two finger-breadths medial and superior to the iliac spine (B) and the second port 8 cm cephalad to the first (C).
Incise the uterus
Infiltrate the uterus with dilute vasopressin (20 U in 60 mL of saline), taking care to administer no more than 10 U at a time to minimize the potential for cardiovascular side effects such as bradycardia and hypertension.14 In the past, we periodically encountered episodes of bradycardia when we used 20 U in 40 mL of saline, but we have not had that problem since we changed to a more dilute vasopressin and used no more than 10 U at a time. It may be that an even smaller amount of vasopressin is just as effective, but we do not yet have sufficient data on myomectomy to determine whether that is the case.
Inject the vasopressin subserosally and along the planned hysterotomy. The fibroid itself contains no blood vessels, but the blood supply to the fibroid generally assumes a coronal pattern around it.15 Therefore, it is important to inject the vasopressin into the correct subserosal plane.
We prefer to make a horizontal hysterotomy using the Harmonic Scalpel (Ethicon Endo-Surgery), but other energy sources, such as a monopolar hook or bipolar spatula, are also appropriate.
We choose a horizontal incision because of the ipsilateral port placement we use for suturing. Surgeons who use a midline or contralateral port for suturing may find it easier to repair a vertical hysterotomy. The pattern of blood vessels along the uterus is heterogeneous and variable, and there is no evidence that blood loss or other outcomes are affected by the direction of the uterine incision.15
Once the uterus has been incised, it is important to work efficiently because bleeding will probably continue until the hysterotomy site is completely closed.
Extract the fibroid ("rock and roll")
Extract the fibroid from the uterus by applying generous traction using a tenaculum, and by applying counter-traction using an atraumatic grasper and the Harmonic Scalpel, as needed. We try to limit the use of thermal energy during this step.
The most important aspect of fibroid extraction is ensuring entry into the correct plane. Appropriate entry makes it possible to remove most fibroids without the need for sharp or thermal dissection.
If you are not sure whether you have entered the correct plane, it is better to cut into the fibroid rather than remain too shallow. If you do not enter all the way into the correct plane, you run the risk of pulling and tearing uterine muscle fibers and causing bleeding.
We describe the technique of fibroid extraction as "rock and roll" because it is generally easier to grab the fibroid near the hysterotomy and roll it out rather than pull on the portion of the fibroid that protrudes from the uterus (see the image, for example).
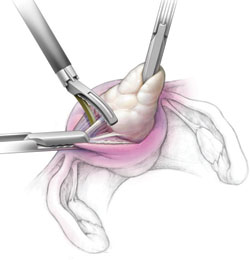
During laparoscopic myomectomy, extract the fibroid by applying generous traction with the tenaculum and counter-traction with an atraumatic grasper and ultrasonic shears. Once you have entered the correct surgical plane, grasp the fibroid near the hysterotomy and simply roll it out of the uterus.
Pregnancy outcomes after laparoscopic myomectomy are generally favorable, with a pregnancy rate that is comparable to or even higher than the rate associated with abdominal myomectomy.1-4
Uneventful vaginal deliveries following laparoscopic myomectomy have been reported in several case series, but so have a number of cases of gravid uterine rupture.5 In a recent study involving 2,050 laparoscopic myomectomies, investigators tracked 386 post-myomectomy pregnancies, 309 deliveries in all, of which 68 were vaginal deliveries.25 It found one case of uterine rupture documented at 33 weeks in a woman who had undergone adenomyomectomy.25
Overall, the literature suggests that uterine rupture after laparoscopic myomectomy is a rare event, occurring in fewer than 1% of pregnancies. Some surgeons use a somewhat arbitrary rule of thumb requiring cesarean delivery if the uterine cavity is entered at myomectomy. This practice is not based on hard evidence, but it does make intuitive sense. If the uterine cavity is entered during myomectomy, it creates a transmural defect that may be more difficult to repair and could carry a higher risk of rupture.
Uterine rupture has also occurred several years after removal of a pedunculated fibroid, suggesting that the use of electrosurgery may weaken the uterine muscle and increase the risk of rupture.
In general—and regardless of the depth of the hysterotomy—it is advisable to counsel patients who have undergone laparoscopic myomectomy that the uterus heals with a scar that may be slightly weaker than the normal myometrium and that elective cesarean delivery may be the optimal strategy. However, a trial of labor is a reasonable alternative, provided the patient receives careful surveillance in a hospital setting.

