For most women, the benefits of initiating a progestin-only or nonhormonal method of contraception at this time outweigh the risks, regardless of breastfeeding status, according to the CDC’s medical eligibility criteria for contraceptive use.6
the patient knows how to use it
The lactational amenorrhea method (LAM) of contraception requires fertility awareness, exclusive breastfeeding, and an ability to recognize the physiologic signs and circumstances that suggest that ovulation is resuming.
How does it work?
Elevated prolactin levels in breastfeeding women inhibit the normal pulsatile secretion of gonadotropin-releasing hormone (GnRH), suppressing the secretion of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the pituitary, thereby inhibiting ovulation (FIGURE).9
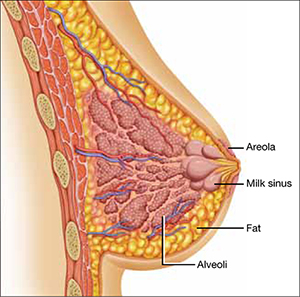
Nipple stimulation from breastfeeding causes the pituitary gland to release prolactin—the hormone that acts at the alveolar secretory cells of the breast to stimulate lactogenesis and at the hypothalamus to decrease the pulsatile release of GnRH. Suckling increases the plasma level of prolactin markedly within 10 minutes of its initiation.
There are three rules for effective use of LAM:
- The infant must be fully or nearly fully breastfed. Prolactin remains elevated for approximately 3 hours, which is about the time it takes for hunger to resume after a feeding of breast milk. Clearly, this level of breastfeeding requires at least one night-time feeding. If cow’s milk formula is given to supplement breastfeeding, its greater fat content slows transit time and prolongs the feeding interval. The result is a decreased prolactin level that may allow FSH and LH to rise and eventually trigger ovulation.
- The woman should be alert for vaginal bleeding after postpartum day 56, which could signal the return of menstruation. The duration of lochia is variable and can make it difficult to detect the onset of menstrual bleeding. In a study by the World Health Organization (WHO), postpartum lochia was present from a minimum of 2 days to a maximum of 90 days, with an average duration of 27 days.10 Most women with LAM will not experience true menstrual bleeding before postpartum day 56 (8 weeks). The frequency of breastfeeding has no effect on the duration of postpartum lochia.
- LAM should be used as contraception only during the first 6 months postpartum. After 6 months, even fully breastfeeding mothers begin to ovulate.
Breast pumping might not maintain an adequate prolactin level
When a woman is separated from her infant, breast pumping has been shown to stimulate the release of prolactin at a level comparable to actual breastfeeding.11 However, women separated from their infant tend to pump less often than they would breastfeed, which can lead to an increased frequency of ovulation and conception.11 Because it is difficult for women to pump at a sufficient frequency to reliably suppress ovulation, the increased risk of pregnancy should be anticipated, and another form of contraception should be encouraged.
What the data show
The WHO conducted a large prospective study examining the relationship between infant feeding and amenorrhea, as well as the rate of pregnancy during LAM. Women who were still breastfeeding and remained amenorrheic had a pregnancy rate of 0.8% at 6 months.10
How the risk of VTE affects the choice of contraceptive
The hematologic changes of normal pregnancy shift coagulability and fibrinolytic systems toward a state of hypercoagulability. This physiologic process reduces the risk of puerperal hemorrhage; however, it also predisposes women to VTE during pregnancy and into the postpartum period. Studies assessing the risk of VTE in postpartum women indicate that it increases by a factor of 22 to 84 during the first 6 weeks, compared with the risk in nonpregnant, nonpostpartum women of reproductive age.7 This heightened risk is most pronounced immediately after delivery, declining rapidly over the first 21 days after delivery and returning to a near-baseline level by 42 days postpartum.
By the time of the recommended 3-week postpartum visit, the period of highest VTE risk has passed. For women who are no longer breastfeeding, the benefits of all hormonal contraceptive methods, including those that contain estrogen, outweigh their risks, according to a newly released update to recommendations from the CDC (TABLE).6 Although combined oral contraceptives are known to increase the risk of VTE by a factor of 3 to 7, data suggest that healthy women who do not have additional risk factors for VTE (e.g., thrombophilia, obesity, smoking, or age of 35 years or older) can use them safely.6
The updated recommendations discourage the use of estrogen-containing contraceptives before 21 days postpartum because they present an unacceptable level of risk (regardless of breastfeeding status), but they allow the use of combined hormonal contraceptives among otherwise healthy breastfeeding women after 30 days postpartum. For women who have additional risk factors for VTE, the risks of combined hormonal contraceptives outweigh the benefits until 6 weeks postpartum, regardless of breastfeeding status.6

