For large areas, bupivacaine 0.25% is utilized, and for small areas, bupivacaine 0.5% is injected into the vulva along with the steroid. The steroid should be drawn into the syringe first (because the vial can be used at a later time), followed by bupivacaine, which is a single-dose vial.
Pudendal nerve blocks using bupivacaine have been helpful in some patients—particularly those who have unilateral pain.
Dr. Gunter: Local injections with a variety of agents for localized, provoked vestibulodynia have been described, including steroids, botulinum toxins, and interferon. It is important to interpret these studies with caution, however, as placebo response rates with injection therapy are significant.25
A retrospective review of submucous injections of methylprednisolone and lidocaine found that 68% of women had a complete or marked response, and two case reports describe success with betamethasone.26,28-30 I offer steroid injections to women who have vestibulodynia before proceeding to vestibulectomy; I find that about 50% get at least partial relief. As Dr. Haefner indicated from her own experience, my success seems best with steroid injections in the vestibule when the painful area is smaller.
Using injectable steroids and botulinum toxins, I estimate that I can prevent 33% to 40% of vestibulectomies. Although this may not be better than the placebo response rate and certainly represents biased patient selection (patients are not required to try local injection before vestibulectomy for vestibulodynia), those who are successful are uniformly happy for trying it, and those for whom it did not work are not unhappy that they “gave it a try,” as these women are all motivated to avoid surgery, if possible.
Pudendal nerve blocks with triamcinolone are also described for women who have generalized unprovoked vulvodynia due to suspected pudendal neuralgia. Ganglion impar blocks—steroid injection around the terminal branch of the sympathetic chain in the presacral space—have also been performed with good results for generalized vulvodynia. I have had good success with pudendal nerve blocks for unilateral pain that is suspected to be pudendal in origin and also with ganglion impar blocks for women with generalized vulvodynia, especially postmenopausal women. I perform all of my own nerve blocks (FIGURE).
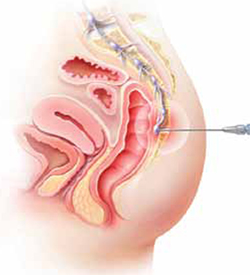
Ganglion impar block
Ganglion impar blocks—steroid injection around the terminal branch of the sympathetic chain in the presacral space—may provide relief from generalized vulvodynia in some women.
Does physical therapy play a role in easing vulvar pain?
Dr. Lonky: What is the role of physical therapy and pelvic floor muscle rehabilitation?
Dr. Gunter: All women who have high-tone pelvic floor dysfunction should be referred to a physical therapist. Many women who lack muscle spasm but experience vulvar pain can still benefit from physical therapy, as gentle stretching and vibration therapy can sometimes be helpful. A physical therapist can also perform biofeedback.
Dr. Edwards: Physical therapy is crucial. It is my first-line therapy overall, with adjunctive oral medication for neuropathic pain. Besides addressing pelvic floor abnormalities, physical therapy can serve as desensitization therapy and psychological support.
Dr. Haefner: Physical therapy has been successful in the treatment of a number of disorders, including migraine and tension headaches, asthma, and anxiety disorders. It is also used in the treatment of vulvar pain. Physical therapists who have experience in vulvar pain may be extremely helpful, particularly if there is concomitant vaginismus—which isn’t uncommon in this population.
For vulvodynia, techniques include internal (vaginal and rectal) and external soft-tissue mobilization and myofascial release; trigger-point pressure; visceral, urogenital, and joint manipulation; electrical stimulation; therapeutic exercises; active pelvic floor retraining; biofeedback; bladder and bowel retraining; and therapeutic ultrasound.
Biofeedback may be used to assist in developing self-regulation strategies for confronting and reducing pain. Patients who have vestibular pain in general have an increased resting tone and a decreased contraction tone. With the aid of an electronic measurement and amplification system or biofeedback machine, an individual can view a display of numbers on a meter, or colored lights, to assess nerve and muscle tension. In this way, she may be able to develop voluntary control over the biological systems involved in pain, discomfort, and disease.
The duration of physical therapy overall and the frequency of visits varies from person to person. Success rates in the range of 60% to 80% have been reported.
How should we respond when medical treatment fails?
Dr. Lonky: What is the proper approach to the patient who has recalcitrant vulvar pain who fails all medical treatments and is not a candidate for vestibulectomy because her pain is outside the vestibule?
Dr. Edwards: The pain clinic. Actually, in a perfect world, the role of the gynecologist or dermatologist would be to give the patient a diagnosis, after which a pain clinic would offer treatment.





