Although the patient in Case 2 has been experiencing migraine with aura for some time without a change in headache pattern, combination hormonal contraception is contraindicated. Her history of migraine with aura may have been missed during previous evaluation if she did not consider it to be a “medical problem.” All candidates for combination OCs should be directly questioned about any history of migraine, thrombosis, cigarette smoking, and hypertension.
The patient described in Case 2 should be encouraged to switch to a progestin-only method of contraception or a highly effective nonhormonal method, such as a copper-containing IUD (Paragard). Because she had no change in her headache pattern on ovulation-suppression therapy (OCs), she likely will have no change with continued ovulation suppression (DMPA, subdermal implant) or without it (LNG-IUS, copper lUD).
Be sure to time the switch in methods so that contraception is maintained throughout the transition. This patient would also benefit from referral to a headache specialist for evaluation and treatment.
CASE 3 Perimenstrual headache in a smoker
A 32-year-old mother of two visits your office for contraceptive counseling. She reports that she smokes two to five cigarettes a day and has a history of migraine without aura. Her headaches occur exclusively during the two days just before her period, and they resolve within the first few days of bleeding. NSAIDs provide limited relief. Is hormonal contraception appropriate?
When a woman with perimenstrual headache is choosing a contraceptive method, we need to ensure that she is not exposed to undue risks and focus on improving her quality of life, if possible.
TABLE 1, reviews the diagnostic criteria for pure menstrual migraine, in which symptoms occur only in the perimenstrual period, as in this patient. Most practitioners use a broader definition of menstrual-related migraine, in which women may have other migraine triggers but still experience predictable headaches with menses. More than 50% of women who have migraine report an association between their headaches and menstruation, but only about 10% of women report migraine exclusively with menstruation.7
Hormonal manipulation is not first-line management for menstrual migraine.19 However, for the patient seeking contraception, it is appropriate to consider the effect of a given method on her headaches because that effect is sure to influence her satisfaction, quality of life, and compliance.
Menstrual migraine is rarely associated with aura, even in women who have migraine with aura at other times in the cycle.7However, the headaches experienced at the time of menstruation tend to be more severe and longer-lasting and less responsive to medication than are migraines experienced at other times of the month.20
Eliminate the placebo week
Research into the pathogenesis of menstrual migraine has focused on the withdrawal of estrogen in the luteal phase of the menstrual cycle. Ovulation is not a requisite for menstrual migraine attacks, which frequently occur during the hormone-free interval in combination hormonal contraceptive regimens. Several lines of evidence suggest that stabilizing estrogen fluctuations can prevent migraine (FIGURE).7
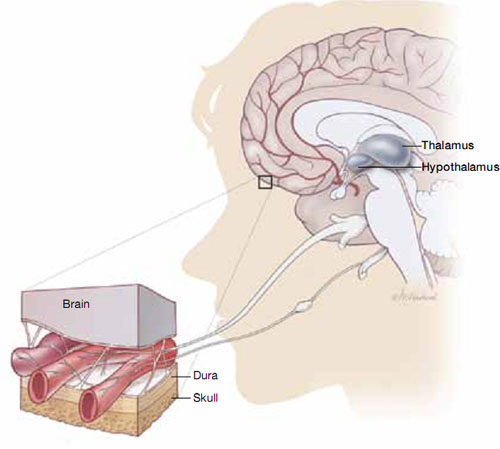
Hormonal fluctuations can trigger migraine
Fluctuations in estrogen during the menstrual cycle may trigger dilation and constriction of blood vessels in the brain, causing migraine.If a patient who has pure menstrual migraine desires to use an estrogen-containing contraceptive, she is likely to be as safe in that choice as a patient without migraine. However, she is not likely to experience improvement in her migraines if she uses a traditional 21/7 active-to-placebo pill regimen. It is necessary to maintain an adequate estrogen level during the placebo week, either through estrogen supplementation or extended-cycle dosing, to prevent the estrogen-withdrawal trigger for headaches.
A few OC regimens reduce the estrogen-free interval to 4 days or provide estrogen supplementation during the placebo week; these regimens may benefit women who have menstrual migraine, although data are scant. If most, or all, of the patient’s migraines are suppressed on combined hormonal contraception, continuous use with rare (e.g., yearly) withdrawals may be indicated.
Alternatives to estrogen-containing contraceptives
If the patient does not desire a combination OC or has other contraindications to estrogen, she may benefit from a progestin-only contraceptive that suppresses ovulation, such as DMPA or the etonogestrel implant. Even with ovulation suppression, however, estrogen fluctuations may occur, and the evidence supporting the use of these methods in the concurrent management of contraceptive needs and menstrual migraine is less clear. Although they are safe in women who have migraine, progestin-only pills and the LNG-IUS do not suppress ovulation reliably enough to be considered useful in managing menstrual migraine.
Take a careful history
Choosing a contraceptive for a woman who has headaches begins the same way as with any other patient: with careful assessment of her short-term and long-term family-planning goals, along with a history and physical to elicit any “red flags,” cultural preferences, and tolerance for specific side effects.

