Botox injection for detrusor overactivity is no quick fix after all
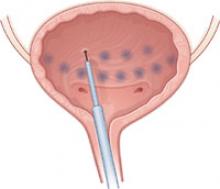
Interest continues to rise in treating detrusor overactivity—with or without incontinence—with botulinum toxin A. Only one commercial product is available in the United States, sold by Allergan under the trade name Botox. Last year, the Pelvic Floor Disorders Network, sponsored by the National Institute of Child Health and Human Development and the Office of Research in Women’s Health, began a placebo-controlled trial of cystoscopic detrusor injection of 200 U of Botox versus placebo, randomized in a 2:1 ratio, for women with incontinence caused by refractory idiopathic detrusor overactivity (FIGURE 2).
Although a sample size of 210 subjects was planned, enrollment was halted after 43 women received injections (28 with Botox, 15 with placebo). The reason: A higher-than-expected rate of urinary retention.
The trial had defined urinary retention as:
- use of catheterization for more than 4 weeks after the date of injection, or
- postvoid residual (PVR) urine of 200 mL or more at the 4-week visit. (The protocol mandated that a patient with this degree of retention be catheterized or that catheterization be considered by the clinician.)
FIGURE 2 Botox relieves detrusor overactivity—but only temporarily
A trial intended to encompass 210 women was halted early because the rate of urinary retention was significantly higher than expected. Twenty-eight women underwent injection of 200 U of Botox, and almost half were classified as having urinary retention 4 weeks after the procedure.
Rate of urinary retention proved to be much higher than anticipated
At the time the study protocol was finalized, most existing studies had focused on patients with neurogenic detrusor overactivity incontinence, many of whom already had impaired bladder emptying treated with self-catheterization. Communication with clinicians using Botox off-label for idiopathic detrusor overactivity incontinence suggested that the occurrence of urinary retention requiring intervention was less than 5%. However, of the 28 women who received Botox, 12 experienced urinary retention; most of these women (9 of 12) had elevated PVR at 4 weeks after injection. Although this elevation was temporary, some women required catheterization for months.
Of the 43 women included in the trial, 12 (28%) experienced urinary retention. However, counting only subjects who received Botox, the proportion with retention was 12 of 28 (43%). None of the women who received placebo experienced urinary retention.
There was also a higher incidence of urinary tract infection in women who developed retention after Botox injection and performed self-catheterization.
Follow-up continues for all 43 subjects, as the protocol provided for monitoring up to 1 year after injection. A full report on the safety and effectiveness of Botox for idiopathic detrusor overactivity in this trial is pending (manuscript submitted for publication).
Catheterization may raise risk of infection without providing a benefit
Ideal management of women who experience elevated PVR after Botox injection is unclear. Many clinicians wonder whether treatment—i.e., catheterization—is necessary for the type of impaired bladder emptying that occurs after Botox injection. It is even possible that catheterization increases the risk of urinary tract infection (or colonization) without providing a benefit to balance that risk.
Botox may still be an option, provided the patient is counseled about risks
Our understanding, albeit incomplete, of the mechanism of action when Botox is used to treat detrusor overactivity does not suggest an increased risk of elevated intravesical pressure leading to ureteral reflux and kidney damage; in fact, normal bladder pressure has been observed in the few studies in which it was measured after Botox injection. However, until we have further information about the short- and long-term risks, if any, of elevated PVR after Botox injection, clinicians should counsel patients about this possibility before proceeding with off-label use of Botox for detrusor overactivity.
Patients unlikely to tolerate repeated Botox injection over several years
Whether or not Botox in its current form will prove to be a useful treatment for women who have detrusor overactivity incontinence remains to be proven conclusively. Even if Botox relieves symptoms, especially in women who have not obtained relief from other treatments, current evidence suggests that the effect is time-limited, probably on the order of several months—although occasional patients obtain relief of greater duration, suggesting an effect that lasts beyond direct Botox action.
Given that most women experience these symptoms on a chronic basis—perhaps especially those who are refractory to usual treatment—it seems unlikely that repeated injections at intervals of only several months can be sustained for years. Ideally, development of second-generation products and further research will produce longer-lasting effects without the need for repeated injections at regular intervals.