In a study of risedronate, 5 mg daily versus placebo, bisphosphonate treatment was associated with a 70% decrease in fracture risk.29
These clinical trials were completed before the development of once-weekly bisphosphonate treatment. Now that such treatment is available, it makes sense to prescribe either alendronate, 70 mg once weekly, or risedronate, 35 mg once weekly. Ibandronate, 150 mg once monthly, is also likely to be effective.
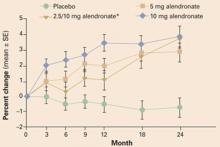
FIGURE 3 Alendronate improves BMD in women taking glucocorticoids
Effects of 2 years of alendronate treatment on bone mineral density of the lumbar spine in patients receiving average daily doses of prednisone of at least 7.5 mg. Alendronate treatment significantly improved bone mineral density (P<.0001). *Alendronate 2.5 mg was switched to 10 mg after it was determined that 2.5 mg was a suboptimal dose.
28 From Adachi JD, Saag KG, Delmas PD, et al. Two-year effects of alendronate on bone mineral density and vertebral fracture in patients receiving glucocorticoids: a randomized, doubleblind, placebo-controlled extension trial. Arthritis Rheum. 2001;44:202–211. Copyright ©2001. Reprinted with permission of Wiley-Liss, Inc., a subsidiary of John Wiley & Sons, Inc.
Do US women get adequate treatment?
Surveys of community-based practices report that approximately 40% of women taking chronic glucocorticoid therapy are not receiving any intervention to prevent osteoporosis.30
Gynecologists are well positioned to ensure that these young women are fully apprised of their options and receive appropriate preventive intervention.
CASE 3 MANAGEMENT
Glucocorticoid-related bone loss
Estrogen-progestin patch, a bisphosphonate, and a rheumatology consult
This patient was started on an estrogen-progestin contraceptive patch and a bisphosphonate. An annual BMD measurement is planned.
In addition, a rheumatologist was consulted to determine if etanercept (Enbrel) could be initiated for the treatment of her rheumatoid arthritis, with a concomitant reduction in her prednisone dosage.
SUMMARYAim treatment toward future bone health
Many controversies remain unresolved concerning the best approach to bone loss in young women. On the one hand, most young women with osteoporosis are at low risk of vertebral and hip fracture, so a large number would need to be treated to prevent one fracture. On the other hand, most hope to become middle-aged; if young women begin adult life with osteoporosis, it is possible that they will have a poor foundation upon which to achieve optimal bone health. Until this key issue is resolved, it is probably best to try to help young women with osteoporosis achieve the best bone health possible. Bone health in young women is likely to be the foundation determining their future bone health and fracture risk.