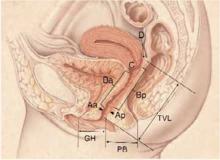
FIGURE 2Quantifying pelvic organ support
Nine sites—points Aa, Ba, C, D, Bp, and Ap; the genital hiatus (GH); the perineal body (PB); and total vaginal length (TVL)—are used to measure pelvic organ support. This drawing represents Stage 0 prolapse, as there is no descent of any of the vaginal compartments. Points Aa and Ap are always measured at the point exactly 3 cm from the reference point of the hymenal ring. Since there is no descent in this example, points Aa and Ap are both -3.
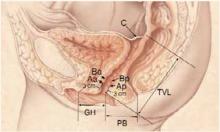
FIGURE 3Posthysterectomy pelvic organ prolapse quantitative (POPQ) examination
POPQ examination for a patient with normal support who has undergone a hysterectomy. When compared to FIGURE 2, notice the absence of point D; point C now represents the vaginal cuff.
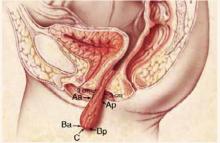
POPQ examination for a patient with vault prolapse after a hysterectomy. Notice how points Aa and Ap are now located outside the body, but are still exactly 3 cm from the hymen. The most distal part of the anterior wall (point Ba), the vaginal cuff (point C), and the most dis-tal part of the posterior wall (point Bp) are all at the same position.
Laboratory studies
Initial laboratory studies should include a urine dipstick analysis and possible culture to evaluate for infection or hematuria. A lower urinary tract infection can produce symptoms such as urgency, frequency, and nocturia, which can mimic the presentation of urge incontinence or interstitial cystitis. Hematuria may herald a more worrisome but rare condition such as transitional cell cancer of the bladder.
Indications for urodynamic testing
Although the basic office evaluation outlined here provides adequate information to properly treat most women with urinary incontinence, further evaluation is appropriate in some cases. A thorough discussion of urodynamics is beyond the scope of this article, but it is important to understand when a patient may require additional investigations. In 1996, the Agency for Health Care Policy and Research recommended further evaluation of patients who:
- Have an uncertain diagnosis
- Fail to respond to treatment
- Are considering surgical intervention, particularly if previous surgery failed or the patient is a high surgical risk
- Exhibit comorbid conditions such as:
- · hematuria without infection
- · voiding dysfunction
- · recurrent urinary tract infection
- · prior anti-incontinence surgery
- · pelvic-organ prolapse beyond the hymen
- · a neurologic condition
Further evaluation may involve simple or complex urodynamics, cystoscopy, and various forms of urinary tract imaging. However, these tests are clearly not necessary for all patients.