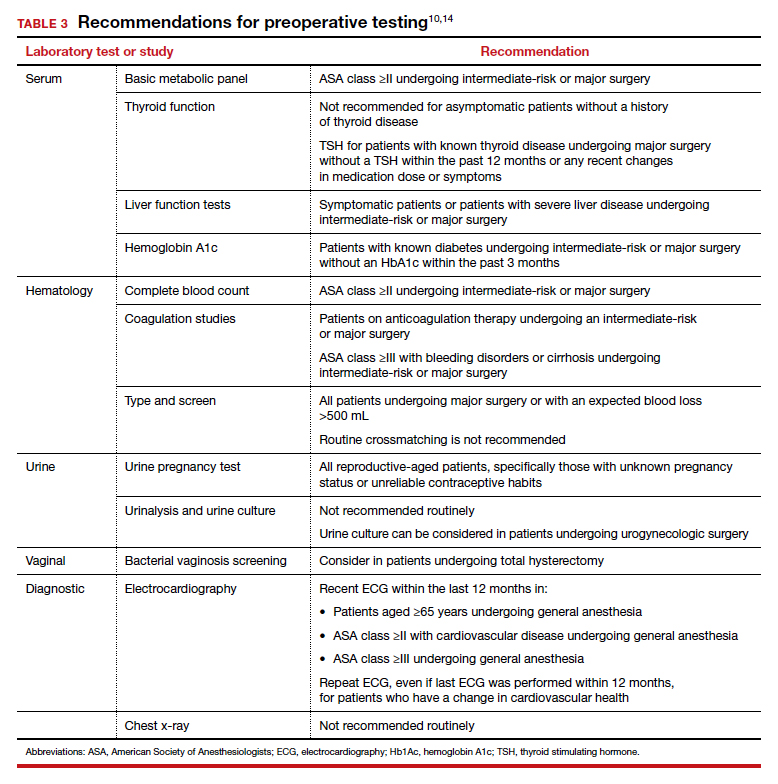
Diagnostic studies
Electrocardiography (ECG). The absolute difference in cardiovascular death is less than 1% among patients with and without ECG abnormalities undergoing a noncardiac procedure with minimal to moderate risk; therefore, routine ECG for low-risk patients should not be performed.23 Instead, ECG should be performed in patients with known coronary artery disease or structural heart disease and in patients aged 65 years and older, since age older than 65 years is an independent predictor of significant ECG abnormalities.24,25 We therefore recommend that the following individuals have an ECG within the last 12 months: patients aged 65 years and older, patients in class ASA II or higher with cardiovascular disease, and patients in class ASA III or higher undergoing general anesthesia. If there is a change in cardiovascular health since the most recent ECG—even if it was performed within 12 months—a repeat ECG is warranted.10,14
Chest x-ray. Despite a high rate of abnormalities seen on routine and indicated chest x-rays, there is no significant difference in perioperative pulmonary complications among patients with a normal or abnormal chest x-ray.16 Rather than changing surgical management, these abnormal results are more likely to lead to the cancellation or postponement of a surgical procedure.7 We therefore recommend against routine preoperative chest x-ray.14
The bottom line
Preoperative testing serves as an additional component of surgical planning. The fact is, however, that abnormal test results are common and frequently do not correlate with surgical outcomes.26 Instead, they can lead to unnecessary surgical procedure cancellations or postponements, undue anxiety in patients, increased liability among physicians, and rising health care costs.5-7
Rather than overly relying on routine laboratory or diagnostic studies, the history and physical examination should continue to be the cornerstone for surgeons responsible for assessing surgical risk. With individualized risk assessment, specific, indicated testing rather than routine nonspecific testing can be obtained.10,14 In short, low-risk patients undergoing noncardiac surgery are unlikely to benefit from preoperative ECG, chest x-ray, or routine laboratory testing without clinical indication. ●