FACTORS TO CONSIDER IN TREATMENT DECISIONS
Although primary care physicians may encounter individuals experiencing their first episode of psychosis, it’s more likely that patients presenting with signs and symptoms of the disorder have been experiencing them for some time and have received no psychiatric care. In both instances, schizophrenia is best managed in conjunction with a psychiatrist until symptoms are stabilized.5 Psychosis does not always require hospitalization. But urgent psychiatry referral is recommended, if possible. Consider admission to a psychiatric inpatient unit for anyone who poses a danger to self or others.8,10
Treatment for schizophrenia is most effective with an interprofessional and collaborative approach that includes medication, psychological treatment, social supports, and primary care clinical management.11,12 The last aspect takes on particular importance given that people with schizophrenia, compared with the general population, have a higher incidence of medical illness, particularly cardiovascular disease.13
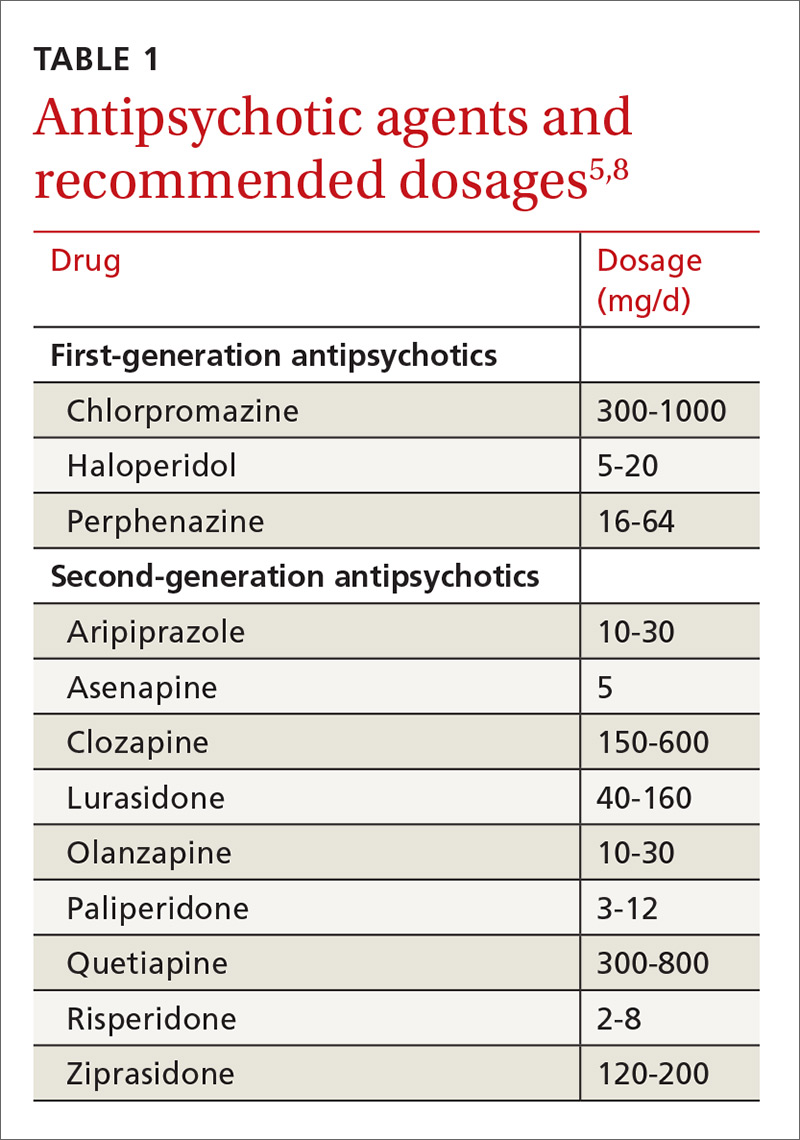
Medications (TABLE 15,8) are grouped into first-generation antipsychotics (FGAs) and second-generation, or atypical, antipsychotics (SGAs), with the 2 classes being equally effective.14-16 Quality of life is also similar at one year for patients treated with either drug class.14
Adverse effects can differ. The main difference between these medications is their adverse effect profiles. FGAs cause extrapyramidal symptoms (dystonia, akathisia, and tardive dyskinesia) more often than SGAs. Among the SGAs, olanzapine, asenapine, paliperidone, clozapine, and quetiapine cause significant weight gain, glucose dysregulation, and lipid abnormalities.5,8,12,17 Clozapine is associated with agranulocytosis, as well. Risperidone causes mild to moderate weight gain.5,8,12,17 Aripiprazole, lurasidone, and ziprasidone are considered weight neutral and cause no significant glucose dysregulation or lipid abnormalities.5,8,12,17 All antipsychotics can cause QT prolongation and neuroleptic malignant syndrome.5,8,12,17
Keys to successful treatment. Antipsychotics are most effective in treating positive symptoms of schizophrenia and show limited, if any, effect on negative or cognitive symptoms.18,19 Give patients an adequate trial of therapy (at least 4 weeks at a therapeutic dose) before discontinuing the drug or offering a different medication.20 All patients who report symptom relief while receiving antipsychotics should receive maintenance therapy.12
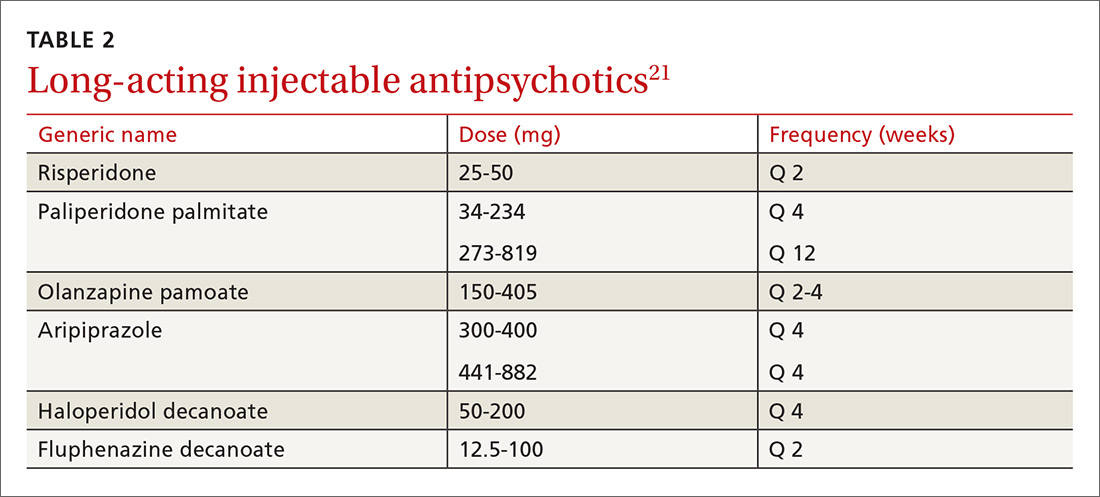
As with all chronic illnesses, success in managing schizophrenia requires patient adherence to the medication regimen. Discontinuation of antipsychotics is a common problem in schizophrenia, resulting in relapse. Long-acting injectable agents (LAIs) were developed to address this problem (TABLE 2).21 Although LAIs are typically used to ensure adherence during maintenance treatment, recent research has suggested they may also be effective for patients with early-phase or first-episode disease.22
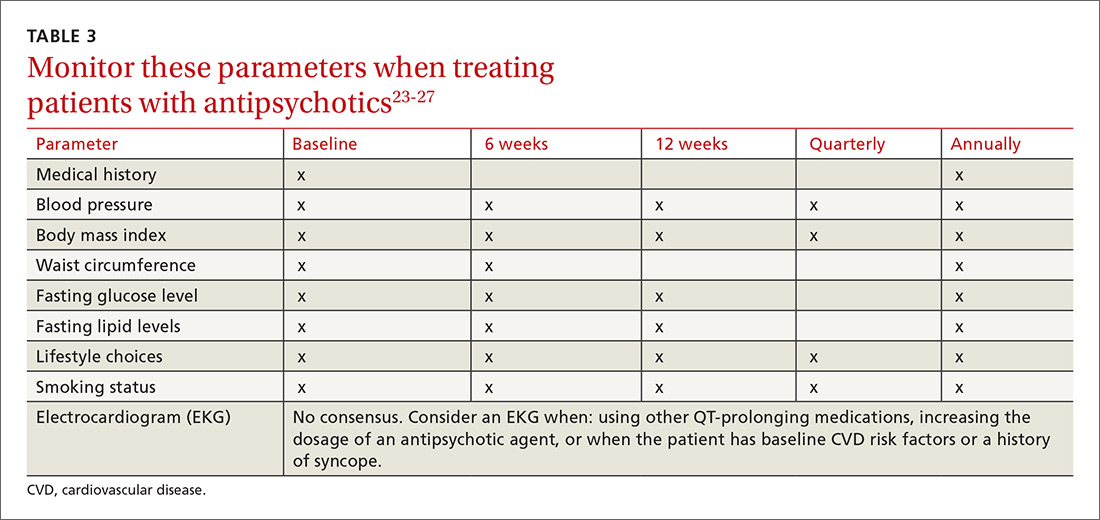
What to watch for. Patients on SGAs may develop metabolic abnormalities, and ongoing monitoring of relevant parameters is key (TABLE 323-27). More frequent monitoring may be necessary in patients with cardiovascular risk factors. Continue antipsychotics for at least 6 months to prevent relapse.12 Also keep in mind the “Choosing Wisely” recommendation from the American Psychiatric Association of not prescribing 2 or more antipsychotics concurrently.28
Adjunctive treatment should also be offered
In addition to receiving medication, patients with schizophrenia should be offered adjunctive therapies such as cognitive behavioral therapy, family intervention, and social skills training.10-12 Among patients with schizophrenia, the incidences of anxiety disorder, panic symptoms, posttraumatic stress disorder, and obsessive compulsive disorder are higher than in the general population.29 To address these conditions, medications such as selective serotonin reuptake inhibitors and anxiolytics can be used simultaneously with antipsychotic agents.
CLINICAL COURSE AND PROGNOSIS CAN VARY
Schizophrenia can have a variable clinical course that includes remissions and exacerbations, or it can follow a more persistently chronic course.
Mortality for patients with schizophrenia is 2 to 3 times higher than that of the general population.30 Most deaths are due to an increased incidence of cardiovascular disease, respiratory illness, cancer, stroke, and other thromboembolic events.30
The lifetime prevalence of suicide attempts among individuals with schizophrenia is 20% to 40%,31 and approximately 5% complete suicide.32 Risk factors include command hallucinations, a history of suicide attempts, intoxication with substances, anxiety, and physical pain.32 Clozapine has been shown to reduce suicide risk and may be considered for patients who are at high risk for suicide.32
Therapeutic response varies among patients with schizophrenia, with one-third remaining symptomatic despite adequate treatment regimens.4
CARE MANAGERS CAN HELP ADDRESS BARRIERS TO CARE
Certain patient, provider, and health care system factors can hamper the provision of primary care to people with schizophrenia. Symptoms of the illness may disrupt the patient’s ability to engage with a provider or clinic. Access to mental health services may be limited based on geography. Even when primary care and mental health services are available, a patient with schizophrenia can find it challenging to schedule appointments. Reducing such barriers by using care managers may be an effective way to improve the overall quality and effectiveness of primary care for patients with schizophrenia.33