THE CASE
A 46-year-old man presented to the emergency department (ED) with sudden-onset right-sided visual loss. He had a history of asthma, but no family history of hypercoagulability, deep vein thrombosis (DVT), or stroke. The patient had an active lifestyle that included scuba diving, mountain biking, and hockey (coaching and playing). The physical examination revealed a right homonymous upper quadrantanopia. The neurologic examination was within normal limits, except for the visual deficit and unequal pupil size. A computerized tomography scan of the patient’s head did not reveal any lesions.
Based on the patient’s clinical picture, the ED physician prescribed alteplase, a tissue plasminogen activator (tPA), and admitted him to the intensive care unit for monitoring.
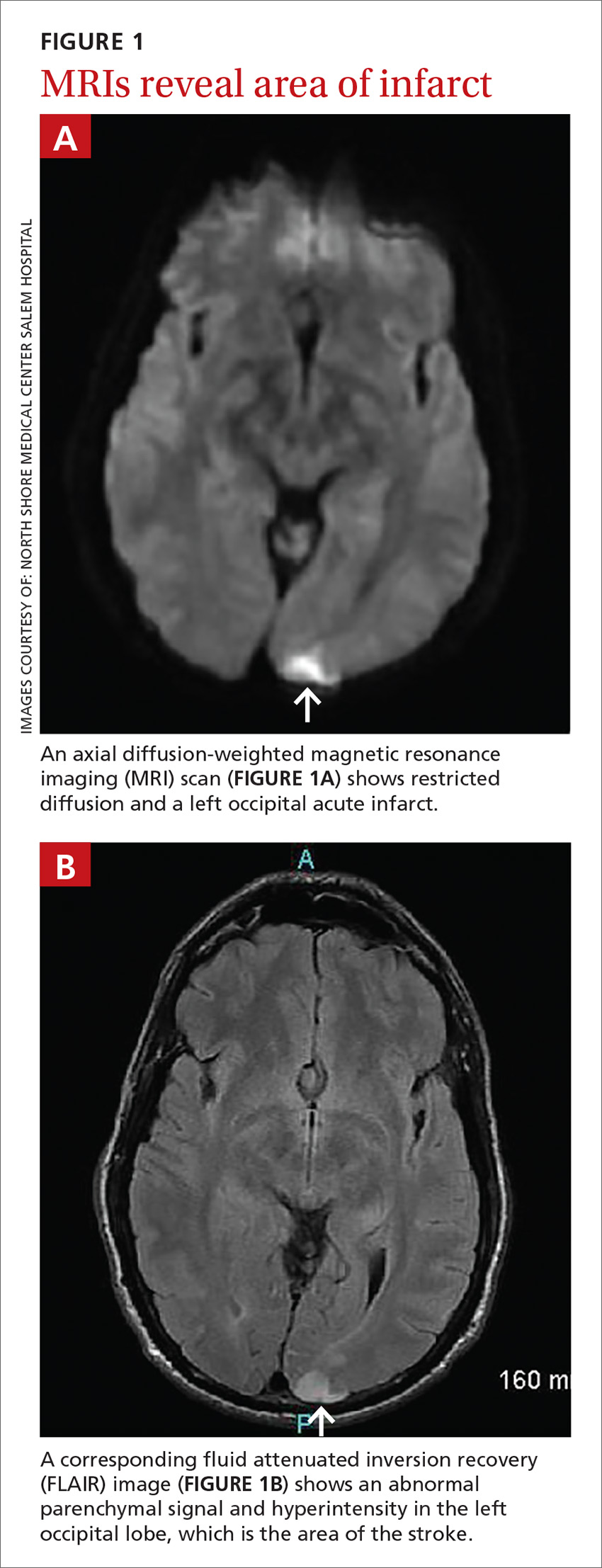
Subsequent magnetic resonance imaging (MRI) of the brain showed multiple small areas of acute infarct in the posterior circulation territory bilaterally, with involvement of small portions of the bilateral cerebellar hemispheres and parts of the left occipital lobe (FIGURE 1A and 1B).
An electrocardiogram showed no evidence of atrial fibrillation, and hypercoagulability studies were within normal limits. There was no evidence of May-Thurner anatomy, and an ultrasound of the lower extremities showed no DVT.
THE DIAGNOSIS
An echocardiogram with bubble study confirmed a diagnosis of patent foramen ovale (PFO) with bidirectional flow, a normal ejection fraction, and no evidence of left ventricular or left atrial thrombus. We started the patient on the anticoagulant enoxaparin 70 mg bid bridged with warfarin 5 mg/d.
Taking the patient’s active lifestyle into consideration, he was approved for PFO closure by the PFO committee and underwent closure. Following treatment, the patient was left with a residual 2-mm blind spot in the right visual field. At a 2-year follow-up visit, he showed no new focal deficits or recurrent symptoms.
DISCUSSION
Since 1988 when Lechat et al reported increased incidence of PFO in young stroke patients,1 many studies have supported the association between PFO and cryptogenic stroke (CS) in young adults.2 Because it remained controversial as to whether PFO is a risk factor for stroke or transient ischemic attack recurrence,3 researchers investigated PFO closure as a preventive measure to decrease stroke recurrence in patients with both CS and PFO.
A 2012 meta-analysis showed possible benefits of closure compared with medical management using antiplatelet or anticoagulation therapies.4 However, these results were not supported by results of other studies. These include the CLOSURE I trial,5 which compared device closure of PFO with medical therapy, and the RESPECT6 and PC trials,7 which did not show a significant difference in the primary end point of recurrent stroke between patients who received medical therapy and those who had PFO closure.
American Heart Association/American Stroke Association’s 2011 guidelines recommend only antiplatelet therapy for patients with CS and PFO.8 While there is consensus that surgical closure is not better than a medical approach to patients with CS and PFO, cases should be individualized, as a patient’s clinical or social factors may dictate otherwise.