We audited reports monthly and provided feedback to the practice team with a written report at the end of each 3-month period starting in June 2013 and ending in June 2014 (5 reports). Individual on-site visits to meet and discuss progress were completed in September 2013 and March 2014, in addition to the initial visit in March 2013.
Evaluation
We compared reported monthly safety events for each of the 6 practices and for the 6-practice collaborative in the aggregate for the 12-month pre-intervention period (April 2012 through March 2013) and post-intervention period (April 2013 through March 2014). Each practice was compared with 3 specialty- and size (number of providers)-matched practices, none of whom received education or feedback on reporting or had patient safety coaches in the practice. In addition, for each of the 3 family medicine practices in the collaborative, we matched 1:3 other family medicine practices for specialty, size, and presence of a designated and trained patient safety coach. For the duration of the project, only 50 of 380 practices in the medical group had a trained patient safety coach.
The rate of safety events reported (ie, number of safety events reported/number of patient encounters) was compared for the 2 time periods using Poisson regression or zero-inflated Poisson regression. SASenterprise guide5.1 was used for all analyses. A P value of < 0.05 was considered statistically significant. The protocol was reviewed by the institutional review board of Novant Health Presbyterian Medical Center and a waiver for informed written consent was granted.
Results
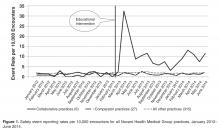
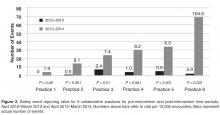
For the year preceding the recruitment and education of the collaborative practices (pre-intervention year), reporting rates for the 6 collaborative practices (1.2 or 19 events reported/154,148 patient encounters) and for the aggregate of 27 comparators (1.5 or 84/568,417) were very similar ( P = 0.47). For the post-intervention year, the collaborative practices’ rate increased to 11.5 (175/152,610, P < 0.001), while the rate for the comparator practices remained stable at 1.5 (81/554,608). Rates remained unchanged as well for all other Novant Health Medical Group practices ( Figure 1 ).Each of the 6 collaborative clinics experienced at least a doubling of reporting rates, and 5 of the 6 clinics significantly increased reporting rates ( Figure 2 ). Practices 1 through 5 had pre-intervention rates of 0 to 2.4 and post-intervention rates of 6.0 to 8.2. Practice 6 increased from 5.9 to 164.6, an increase largely due to reporting of communication issues for this practice. In practice 1, a general surgery practice, reporting increased from 0 events (in 5093 encounters) to 4 events (in 5071 encounters, a rate of 7.9) for the 2 time periods. However, this increase did not reach the level of significance ( P = 0.09). The 3 general surgery clinic comparators together reported 0 safety events for the post-intervention year among 13,793 encounters in clinic.To control for the presence of patient safety coaches in practices, the 3 family medicine clinics (clinics 4 through 6, Figure 2) were each matched 1:3 for size (number of providers) and specialty (other family medicine clinics), also with a patient safety coach. While the rates were significantly increased for the 3 collaborative family medicine clinics ( P < 0.001), only 1 of the comparators clinic’s rate changed significantly (0.2 or 1/44,580 to 1.3 or 6/45,157), and this change was marginally significant ( P = 0.048). This practice was the only one of the 27 comparator clinics to demonstrate any increased rate.