In this article, we first summarize the background and methodology of the Perfect Depression Care initiative. We then describe the application of this methodology to spreading Perfect Depression Care into 2 nonspecialty care settings—primary care and general hospitals. Finally, we review some of the challenges and lessons learned from our efforts to sustain this important work.
Building a System of Perfect Depression Care
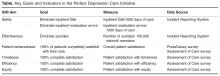
The bedrock of Perfect Depression Care was a cultural intervention. The first step in the intervention was to commit to the goal of “zero defects.” Such a commitment is not just to the goal of improving, but to the ideal that perfect care is—indeed, must be—attainable. It is designed to take devoted yet average performers through complete organizational transformation. We began our transformation within BHS by establishing a “zero defects” goal for each of the IOM’s 6 aims ( Table). We then used “pursuing perfection” methodology to work continually towards each goal [5].One example of the transformative power of a “zero defects” approach is the case of the Effectiveness aim. Our team engaged in vigorous debate about the goal for this aim. While some team members eagerly embraced the “zero defects” ambition and argued that truly perfect care could only mean “no suicides,” others challenged it, viewing it as lofty but unrealistic. After all, we had been taught that for some number of individuals with depression, suicide was the tragic yet inevitable outcome of their illness. How could it be possible to eliminate every single suicide? The debate was ultimately resolved when one team member asked, “If zero isn’t the right number of suicides, then what is? Two? Four? Forty?” The answer was obvious and undeniable. It was at that moment that setting “zero suicides” as the goal became a galvanizing force within BHS for the Perfect Depression Care initiative.
The pursuit of zero defects must take place within a “just culture,” an organizational environment in which frontline staff feel comfortable disclosing errors, especially their own, while still maintaining professional accountability [6]. Without a just culture, good but imperfect performance can breed disengagement and resentment. By contrast, within a just culture, it becomes possible to implement specific strategies and tactics to pursue perfection. Along the way, each step towards “zero defects” is celebrated because each defect that does occur is identified as an opportunity for learning.
One core strategy for Perfect Depression Care was organizing care according to the planned care model , a locally tailored version of the chronic care model [7]. We developed a clear vision for how each patient’s care would change in a system of Perfect Depression Care. We partnered with patients to ensure their voice in the redesign of our depression care services. We then conceptualized, designed, and tested strategies for improvement in 4 high-leverage domains (patient partnership, clinical practice, access to care, and information systems), which were identified through mapping our current care processes. Once this new model of care was in place, we implemented relevant measures of care quality and began continually assessing progress and then adjusting the plan as needed (ie, following the Model for Improvement).