In this article, we describe the project and effects on diabetes-related clinical health outcomes.
Methods
Setting
Whittier Street Health Center (WSHC) is a federally qualified community health center that serves over 25,000 patients annually. The WSHC is situated in the heart of Boston’s Roxbury neighborhood, close to 5 public housing developments; 83% of WSHC patients live in public housing units. Roxbury is an underserved neighborhood with high rates of poverty, violence, and disease [12]. African Americans comprise the majority of residents living in Roxbury, making up 55.6% of the total population [13].
Diabetes Care Coordination Program
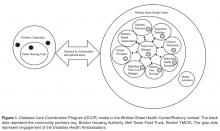
The DCCP took place from December 2011 to June 2013. The DCCP team provided diabetes self-management education, support, and comprehensive diabetes care using the patient-centered medical home (PCMH) model [14] and Diabetes Health Ambassadors as mediators for program delivery ( Figure 1 ). Team members included: 1) a patient navigator (BA degree and completed an 8-week patient navigator course at the health department), 2) a diabetes nurse case manager, 3) certified diabetes educator, 4) a registered dietitian, 5) a clinical pharmacist, 6) an integrated behavioral health specialist, 7) a primary care physician, 8) an outreach nurse, 9) Diabetes Health Ambassadors, 10) a high-risk nurse case manager, and 11) a program manager. All team members were already working within the medical home except the patient navigator, outreach nurse, and the Diabetes Health Ambassadors. Clinical team members already working at WSHC worked on this project for half of their total hours and sometimes more based on patients’ needs for the duration of this project.Ambassadors
Diabetes Health Ambassadors, a key component of the program, were hired to engage community members in managing their own health. Five Ambassadors were recruited and retained throughout the project period. Ambassadors were referred by their primary care provider at WSHC and interviewed for the job by the patient navigator. Ambassadors were required to be African-American women with type 2 diabetes living in a public housing unit within the Roxbury neighborhood. In addition, they were required to have their diabetes under control as defined by the WSHC clinical team (HbA1c of 8.0 or below). They also had to want to help other women control their diabetes and be able to deliver motivational presentations as well as have knowledge of available community resources.
Ambassadors received 30 hours of paid training from the certified diabetes educator. During training, they learned the definition, risk factors, and causes of diabetes, how it is controlled, and how to explain this information at a fifth-grade level. Modeling and feedback was used to assure that the information each Ambassador presented was accurate. Ambassadors were also trained on how to measure blood pressure and blood glucose levels and how to respectfully deliver the results. Additionally, Ambassadors received training on cultural competence. Ambassadors were engaged in community outreach and patient support for 20 hours per week and were compensated for their time with stipends.
Participant Recruitment and Outreach
A rolling enrollment for the DCCP began January 2012. The outreach team from the WSHC attended coffee hours at the public housing units and other community events where they conducted onsite blood pressure and glucose screenings as well as educated community members on healthy eating and active lifestyle to reduce the risks for diabetes. Mobile kits were used for testing, so participants received the test results immediately. Two Ambassadors, the outreach nurse, and the patient navigator conducted the outreach events. The set up included two tables, 6 chairs, education materials, and blood pressure and blood sugar screening materials.