Recognizing and overcoming practice-specific barriers to vaccinating adults are needed to improve uptake. A lack of patient- and provider-focused reminders may lead to missed opportunities to vaccinate [11,12]. Provider and patient-focused reminder tools can be effective in increasing vaccine uptake [1,13,14], but interventions that combine reminder tools with patient outreach may be more effective [15]. Furthermore, involving an interdisciplinary team to coordinate the administration of vaccines among adults may improve vaccine uptake rates [16]. These studies suggested the need to determine a standard, effective reminder tool and incorporate multilevel interventions to increase uptake of adult vaccines.
An informal electronic query at a large, suburban family practice revealed approximately 30% Tdap and PPSV coverage rates among eligible adults served by the practice, suggesting that providers fail to assess patients’ vaccine status at every opportunity. Electronic medical records provide no alerts for vaccines that may be due. PPSV and Tdap uptake rates were chosen for this quality improvement project to address low baseline coverage rates among adults. The objective of this project was to increase adult Tdap and 23-valent PPSV uptake rates using a reminder checklist at the point of care. A secondary objective was to assess providers’ vaccination practices during various types of visits, appraise their perceived vaccination practices and barriers to vaccinating adults, and to determine providers’ perceived effectiveness of the reminder checklist.
Methods
This quality improvement project was implemented in a large family practice that is home to a family medicine residency program. Approximately two-thirds of the patients served are adults, over half of whom are minorities, and nearly half are on Medicaid or underinsured. Providers in the practice included 21 resident physicians, 8 attending physicians, and 1 nurse practitioner who served as the primary investigator. Institutional review board approval for this study was obtained.
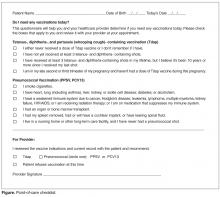
A vaccine checklist was initiated at the point of care to serve as a vaccination reminder to both providers and patients. The checklist was adapted with permission from “Do I Need Any Vaccinations Today?” [17, Figure]. The checklist was intended to be distributed by the front desk staff to anyone in the targeted age-group (adults, 18–64 years) who presented for an office visit. The front desk staff asked these patients to complete the checklist and discuss it with their provider at their appointment. This intervention continued for 3 months. Prior to initiating the intervention, the providers and front desk staff were educated about the use of the checklist; however, not all providers and front desk staff were present for the formal education and relied on other staff educating them as the intervention was implemented.Measures included pre- and post-intervention vaccination rates for Tdap and PPSV, the providers’ perceived vaccination practices during various types of visits, the providers’ perceptions of practice-specific barriers to vaccinating adults, and the providers’ perceived usefulness of a vaccine checklist. To evaluate the effect of the reminder tool on immunization rates, we conducted a chart review. A random sample of 30 charts was derived separately for each vaccine, pre- and post-intervention, by selecting every 5th chart via the electronic health record after filtering for vaccine eligibility. Eligibility for the vaccines was based on age, vaccine history, and diagnoses noted in the medical history and problem list.