For the period October–December 2014, we tabulated 231 near-miss wrong-patient orders that occured throughout the health system, of which 37% occurred in the ED. This translated to about 1 near-miss event per day in the ED. Given this data, the ED was the location for our quality improvement project.
Intervention
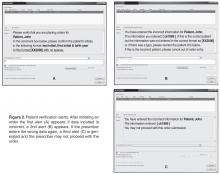
We implemented an ID reentry function in the CPOE system that prompts the prescriber to enter the patient’s initials and year of birth at the beginning of the order entry session ( Figure 2A ). This active double identification system is in line with the Joint Commission’s National Patient Safety Goal of using at least 2 patient identifiers when providing care, treatment and services. If the prescriber correctly inputs this data, then the ordering process can proceed. If the data is incorrect, then a second alert is activated ( Figure 2B ), allowing for correction of typographical errors that may not be related to an actual patient ID error. If at this point the prescriber enters the correct patient identifier, then he or she can proceed normally with the order. However, if the prescriber enters the wrong patient information again, a third and final alert is generated ( Figure 2C ). The EHR system recognizes this 2nd patient ID error as a true error and will not allow the prescriber to proceed with the order.Outcomes
After a beta testing period of 1 week, the system was implemented on 3 November 2015. To assess the effectiveness of the alert system to prevent ordering errors, we used the retract and reorder tool to measure the rate of wrong-patient order entries for the 8-week period November–December 2015 and compared this with the preimplementation rate. Prior to the intervention, the average number of wrong patient order entries in the ED was 6.125 events per week. After implementation, the average number decreased to 4 events per week, a 35% decrease, and the proportion of near-miss ID errors in the ED relative to all such errors within the health system decreased from 37% to 19%.
Discussion
The original aim of the project was to decrease “wrong patient, right order” near-miss events by 30% in 3 months in the ED using an order-based patient ID reentry function. The goal was rapid improvement using a hard-wired EHR process, which is why a 3-month time frame was chosen. During our 8-week project, we surpassed this goal, documenting a 35% decrease in near-miss wrong-patient orders in the ED. This rate was similar to that achieved by Adelman et al [8] and Green et al [10]. Adelman et al found a 41% error reduction, while Green et al found a short-term 30% reduction in CPOE wrong-patient orders utilizing a 2.5-second mandatory delay before continuing the order entry for the purposes of patient verification.
Resident and attending staff conveyed to us anecdotally during both beta testing and implementation that the ID reentry function made them aware of incorrect patient selection even before entering the required initials and birth year. They then cancelled the order session on the wrong patient and chose the correct patient. This is consistent with the findings of Green’s study, which noted that ED practitioners backed out of appropriately 1 in 200 order entry sessions due to wrong patient selection [10].