Addressing Physician Burnout in Pulmonology and Critical Care in Pulmonology and Critical Care
Kelly Vranas, MD, MCR
Assistant Professor of Medicine
Division of Pulmonary, Allergy, and Critical Care Medicine
Oregon Health & Science University;
Critical Care Health Services Researcher
Portland VA Medical Center
Portland, OR

Slideshow below.
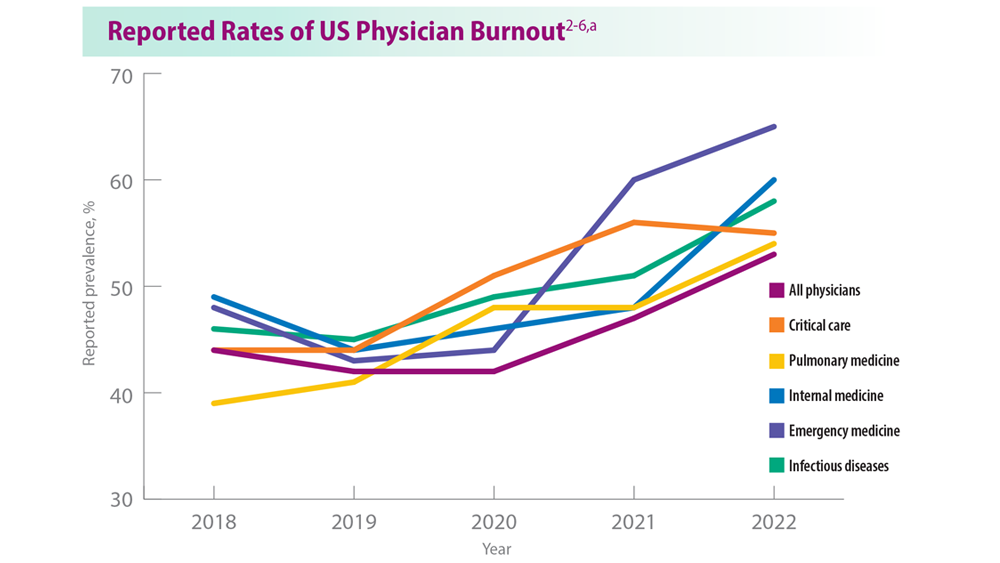
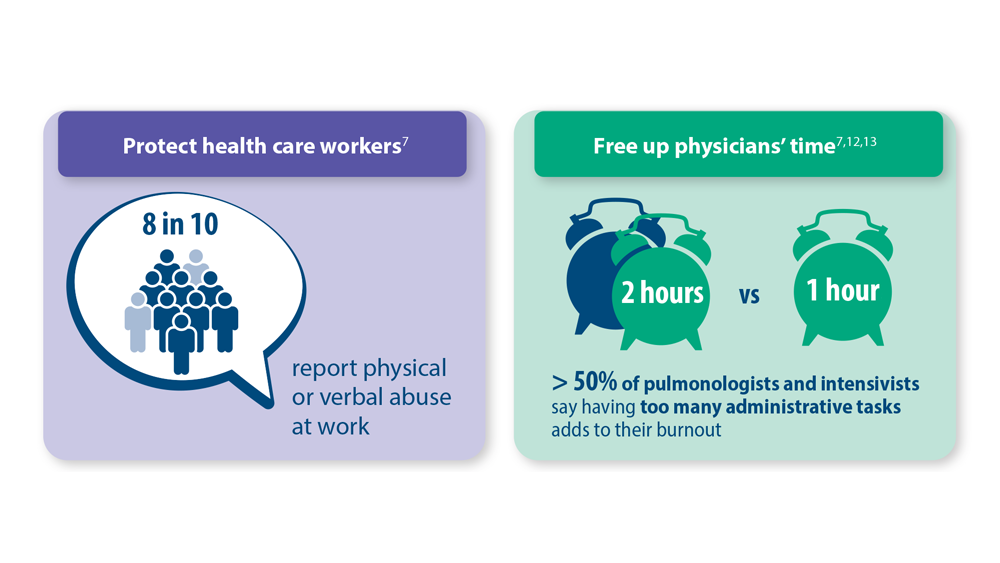
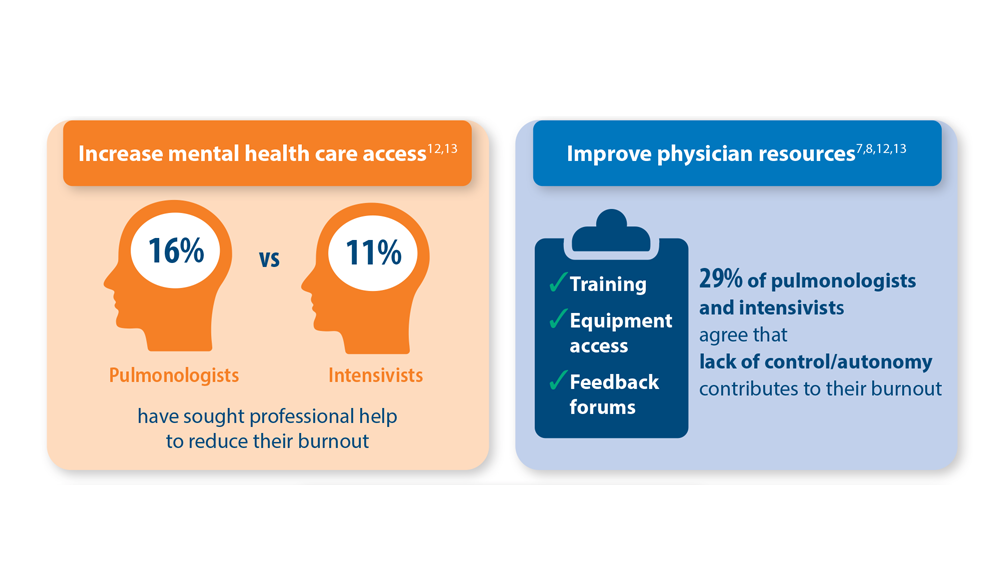
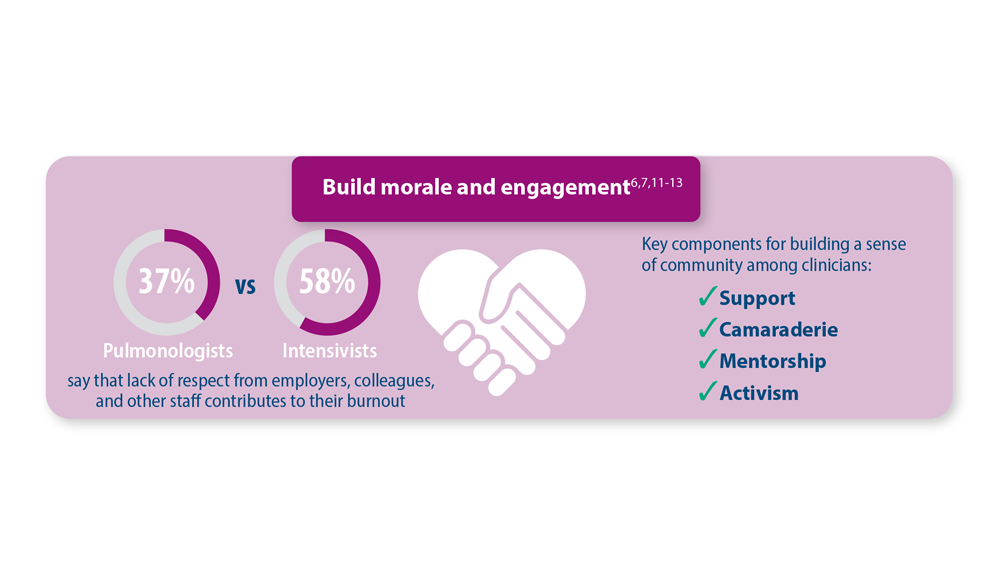
Work-related stress has long been a concern for those working in the intensive care unit (ICU); even before the COVID-19 pandemic, it was estimated that up to 45% of critical care physicians had at least one symptom of severe burnout.1-6 In 2020 and the years following, the combination of significantly increased patient morbidity and mortality rates, excessive workloads, and resource limitations negatively impacted employee morale, decreased feelings of professional fulfillment, increased moral distress, and most importantly, heightened mental health concerns among critical care physicians.7-10
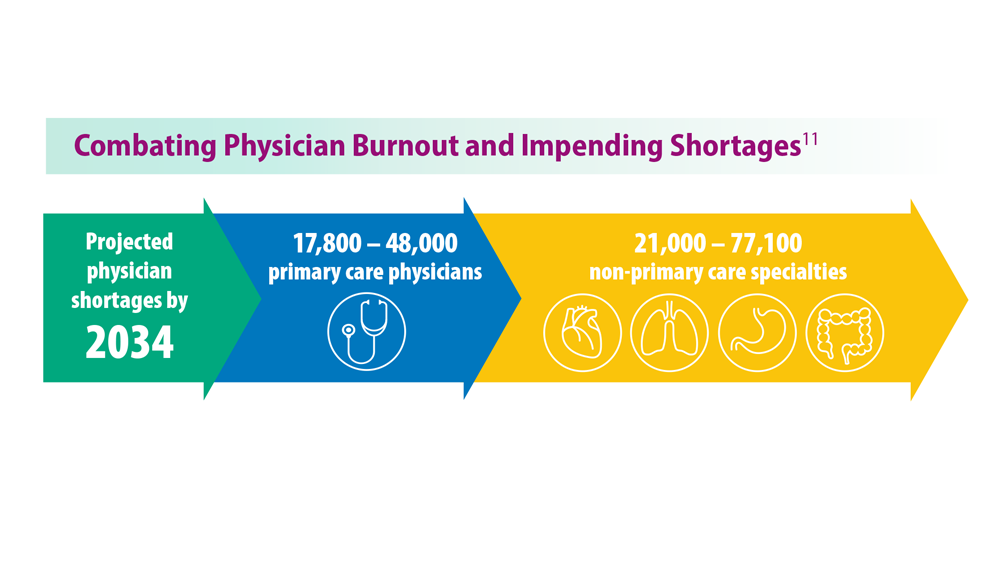
While most of the post-pandemic world has returned to “normal,” its effect on the health care industry has been slower to wane; in fact, reported rates of physician burnout remain higher today than they were in 2020.2-6 Almost half of physicians (49%) say their depressions affects their patient interactions, while 65% report that their personal relationships are affected.6 In order to course-correct—not only for the sake of our current workforce and patients, but also to ensure better preparation for future public health crises—we must address the more fundamental burnout contributors that the pandemic only amplified.
1