This month’s contribution by Gellad et al concerns efficiency within an endoscopy unit. There are over 5,400 Medicare-certified ambulatory surgical centers (ASC) in the United States providing a distributed network of high-quality, accessible centers for patients in need of outpatient endoscopic procedures. Most of these units are running efficiently with little room for waste (or they would not be able to survive in the current environment). Dr Gellad and colleagues have developed a process to analyze efficiency by defining performance metrics based on standard Donabedian analysis. Their article relates mostly to units performing a mix of procedures – usually within a hospital unit. These units, unlike ASCs, deserve our scrutiny since many are operated at efficiency levels that provide "opportunities."
John I. Allen, MD, MBA, AGAF, Special Section Editor
As in other fields of medicine, gastroenterology must now adapt to widespread reform designed to cut costs while maintaining quality. Reimbursement for endoscopy continues to decrease year by year, and the Patient Protection and Affordable Care Act incentivizes high-value health care through value-based purchasing.1 Because gastrointestinal procedures make up the largest percentage of ambulatory surgical center claims in Medicare, value-based purchasing especially will impact gastrointestinal endoscopy units.2
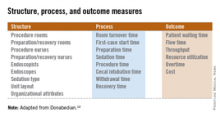
In meeting these challenges, gastroenterologists must evolve in how they manage costs not only to contribute to a healthier national economy, but also to maintain high standards of care in a rapidly changing environment. To do so, clinical efficiency must be monitored with reliable metrics to inform decision making and pinpoint areas in need of improvement. This article reviews the importance of value measurement in endoscopy, develops a conceptual framework for endoscopic efficiency, and proposes key operational metrics for endoscopy unit efficiency.
Value matters
Health expenditures in the United States grew from 5.1% of the gross domestic product in 1960 to more than 17% in 2009.3 Continued growth at this rate is unsustainable and the focus of health care reform has shifted from improving quality alone to optimizing value.4
In health care, value represents outcomes achieved per dollar spent and thus encompasses consideration of both quality and cost.5 In the decade since endoscopic quality measures first were proposed,6 a great deal of discussion has focused on the scientific merit and feasibility of endoscopic quality metrics. In contrast, very little attention has been paid to quality’s companion in the value equation, namely cost. Indeed, although endoscopic practices need to show value through improved quality, decreasing costs through improved efficiency is also critically important.
Furthermore, improved efficiency in endoscopy is not just a business mandate, it is also a quality imperative. In its definition of quality of care, the Institute of Medicine includes timeliness and efficiency as key dimensions of quality.7 Improving efficiency heightens quality while lowering costs, thus making it an ideal target for improving value.
Improving value through improved efficiency
Unfortunately, to borrow a term from our field, the modern health care system is extraordinarily bloated. The Institute of Medicine estimates that $750 billion is lost to inefficient health care spending each year.8 Much of this inefficiency results from the overuse of expensive testing, including endoscopic services. In fact, in its "Choosing Wisely" campaign (www.choosingwisely.org/) the American Board of Internal Medicine, supported by the American Gastroenterological Association, identified endoscopic overuse in three of its five gastroenterology recommendations.9
In addition to overuse of testing, there are a number of other challenges to health care efficiency, including weak inventory management and inefficient use of expensive resources including space, equipment, and staff.5 Although these challenges may be more easily manageable in the small ambulatory surgical center setting, they become exponentially more difficult to overcome in larger, more complex, health system environments such as academic medical centers and large health systems.
Developing efficiency metrics, identifying benchmarks, and providing access to shared data through registries are key steps in addressing these challenges. The accurate measure of efficiency enables health services research and institutional quality control. With reliable efficiency metrics, researchers also can better test interventions to improve value by monitoring their effect on indicative parameters. Similarly, the ability to gauge process and outcome measures will allow institutions to benchmark their practices to best performing peers. Within gastroenterology, registries that contain operational metrics would be an invaluable tool for process improvement.
Conceptual framework for endoscopic efficiency
Effective measures for efficiency across health care generally have not yet been developed.10 The Agency for Health Care Research and Quality (AHRQ) has identified four characteristics of ideal efficiency measures: 1) important: measures should have relevance to key stakeholders such as providers, patients, and policy makers, and be under the control of those stakeholders; 2) scientifically sound: measures should have face, construct, and predictive validity, and be reliable and reproducible; 3) feasible: measures should not require excessive cost or burden to obtain; and 4) actionable: measures should lead to measurable change in a system.11