This article, by Dr. John Inadomi and colleagues is part of the AGA’s process for developing guidelines. The importance of guidelines has increased considerably over the last 25 years. In the first wave of managed care, we were practicing with few if any clinical guidelines. Now, as we move forward toward a value-based reimbursement system, the need for evidence-based practice is paramount. Dr Inadomi and the AGA Clinical Practice and Quality Management Committee have fine-tuned this process over the last 3 years and now describe their results. While many guidelines are labeled as "GRADE," some are simply opinion documents designed with GRADE wording. A fully implemented GRADE process involves rigorous analysis of published data, input from trained GRADE methodologists, and opportunities for both public and expert comment from all involved stakeholders.
John I. Allen, MD, MBA, AGAF Special Section Editor
The economic foundation upon which U.S. health care delivery is built is shifting rapidly. Specifically, reimbursement is changing from fee for service to value-based payments. These include bundled payments for episodes of care, and payments tied to health outcomes with shared reimbursement in which payments are distributed among all stakeholders including primary care, specialty physicians, and hospital systems. Under bundled reimbursement, payments are established a priori for each episode of care, payments will be risk adjusted, and reimbursement will not increase based on the quantity of services provided. Most importantly, payment will be modified based on providers documenting their success in achieving high-quality health outcomes and patient satisfaction compared with similar facilities servicing similar patients.
We are moving rapidly to value-based reimbursement and such changes no longer require the federal government to continue transformation of the health care landscape. In 2009, Blue Cross Blue Shield of Massachusetts compared costs and quality between traditional fee-for-service and a global payment system (the Alternative Quality Contract) whereby participating provider organizations assumed accountability for spending, but also received bonuses for quality.1 Geisinger Health System, an integrated delivery system comprising hospitals, outpatient facilities, and community practices including both employed and affiliated primary care and specialty physicians, now treats 20% of total physician compensation as variable and directly dependent on annual individual and group performance.2
Based on these developments, the most important issue to address is how health care quality is defined. Traditionally, metric development and validation have been the purview of administrators. It is the premise of the AGA Institute that physicians who provide services should lead efforts to define metrics by which our clinical services and health care outcomes are judged. To achieve this goal, the AGA has changed how clinical practice guidelines are constructed and has developed the "Roadmap to the Future of GI Practice," a coordinated program that links guidelines to clinical decision support tools, performance measures, the infrastructure by which clinicians can report their practice outcomes (the AGA Digestive Health Outcomes Registry), the Digestive Health Recognition Program, Practice Improvement Modules, and American Board of Internal Medicine Maintenance of Certification. This article, the first of two that focus on the AGA’s process for guideline development, will summarize the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) methodology to determine the quality of evidence and the strength of recommendations for the AGA’s guidelines.
Guideline development begins with solicitation of topics from AGA members, the AGA Council, and the AGA Clinical Practice and Quality Management Committee (CPQMC). The CPQMC, with guidance from the AGA Council, develops focused clinical questions for each guideline that are submitted to the AGA Governing Board for consideration. For topics approved by the Governing Board, the CPQMC identifies two content experts and one methods expert to author technical reviews, which represent the evidence basis for guideline recommendations. The guideline itself is written by a separate panel that is constructed to provide representation from all stakeholders involved in the care of patients related to the guideline topic.
The AGA Ethics Committee vets potential authors and guideline panel members to identify conflicts of interest and ensure transparency of the process.
GRADE
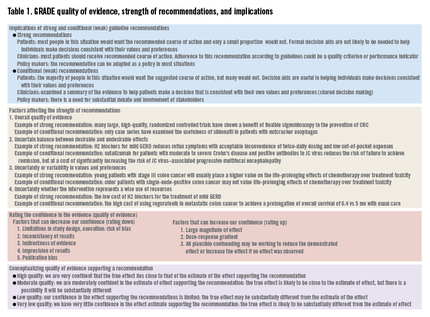
To impact medical practitioners, guidelines must be derived from well-constructed studies from which information can be derived to support clinical recommendations. Because published studies vary in their methods, comparison populations, and statistical strength, some commonly accepted process is needed so that clinicians can determine how reliable guideline recommendations would be. Currently, the most common methodology to judge strength of evidence (and hence strength of our recommendations) is the GRADE framework,3 an internationally recognized method implemented by more than 70 organizations. Importantly, this process is accepted by the National Quality Forum, which is the body responsible for vetting quality metrics that may be adopted by the Center for Medicare and Medicaid Services for use in enhanced reimbursement.