The Medicare Physician Feedback Program provides physicians with comparative information about the quality and cost of care delivered to their Medicare fee-for-service patients through feedback reports known as Quality Resource and Use Reports (QRUR).
Why are QRURs important?
The Patient Protection and Affordable Care Act (PPACA) directed the Health and Human Services Secretary to develop and implement a budget-neutral payment modifier that will adjust Medicare physician payments based on the relative quality and costs of care provided. Quality and cost measures will be risk adjusted, geographically standardized, and should promote systems-based care. The Medicare Physician Feedback Program serves as the foundation for the modifier.
In the 2013 Medicare physician fee schedule final rule published in November of 2012, the Centers for Medicare and Medicaid Services (CMS) announced the first phase toward implementation of the value-based payment modifier. Initially, the value modifier will be applied to group practices of 100 or more eligible professionals – about 1,100 groups nationally. These groups will be able to elect how their payment modifier will be calculated. This will affect payment in 2015 based on 2013 performance. Smaller groups of 2-99 eligible professionals will remain unaffected during the first reporting year. However, CMS is required by statute to apply the modifier to all physicians by 2017. In the future, CMS will be using QRURs to provide all physicians with information about how the value modifier will affect their payment.
The QRURs provide comparative quality and cost data for quality improvement purposes. This is the first time that many physicians will have seen such performance information from CMS. The report previews quality and cost measures that will be used in the value modifier. The report can count as one of the group options to fulfill the Physician Quality Reporting System (PQRS) requirement for group reporting and also for the value modifier.
How will QRURs impact the value modifier?
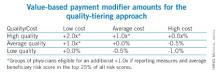
Groups of physicians with 100 or more eligible professionals will have the option of either zero adjustment, a minus one adjustment, or will elect quality tiering calculation based on their PQRS participation. To be a successful PQRS reporter, groups must have registered and will report at least one measure for the Group Practice Reporting Option (GPRO) Web interface, CMS-approved registries, or the administrative claims option that includes administrative claims performance, quality performance measures that will be calculated by CMS. These groups will have the option of having zero adjustment for the value modifier applied to them or the option to elect a quality tiering calculation in which there would be an upward or a downward adjustment (or no adjustment) based on the quality tiering.
Overview of how CMS will calculate the value modifier
Groups that decide that the amount of downward adjustment is not worth the effort or do not wish to participate in PQRS reporting will be considered non-PQRS reporters. Non-PQRS reporters will be subject to a minus 1% downward adjustment of the value modifier and a minus 1.5% downward adjustment for PQRS; note that the amount of downward adjustment is additive for the two programs.
For the value modifier, physicians elect one of three possible group practice options. One option is the Web-based interface that is largely primary care and preventive measures. The second option is to select measures from a registry. The third option is the administrative claim option calculated by CMS. For the first two options, physicians choose which option for quality measures goes into the quality composite of the value modifier. Physicians who choose the administrative claims method are not allowed to choose which measures will be examined for the value modifier.
How is the value modifier calculated?
The value modifier is calculated at the group or taxpayer identification number (TIN) level. The attribution method focuses on the delivery of primary services through a two-step process. The first step identifies whether a physician is in primary care. Beneficiaries are attributed based on those who have had at least one primary care physician (PCP) in service. CMS then examines whether the PCP(s) delivered the plurality of care. The second step checks if the TIN provided the plurality of the primary care services by nonprimary care physicians.
There are five cost measures grouped into two domains: total overall cost or the total per capita measure. The reports examine the total cost of beneficiaries with specific conditions including chronic obstructive pulmonary disease, coronary artery disease, diabetes, and heart failure. Each measure within each domain is weighted equally and each domain is weighted equally to form a cost composite.