Rosai Dorfman disease (RDD) is a rare non-Langerhans cell histiocytosis first described in 1965 by Destombes and again in 1969 by Rosai and Dorfman to depict patients who presented with massive cervical lymphadenopathy.1 The classification for histiocytosis was revised in 2016 based on new insights into the pathologic, genetic, and molecular features of RDD.2,3 Now, RDD is listed under the R group, which includes familial, sporadic, classical (nodal), extranodal RDD, and other noncutaneous, non-Langerhans cell histiocytosis.3 Cutaneous RDD is classified under the C group and typically presents as painless papules, plaques, or nodules without significant lymphadenopathy, or systemic symptoms usually seen in the presentation of RDD.4
The etiology of RDD is poorly understood, although an underlying infectious or genetic component is suspected.5 Several pathogens—including human herpesvirus 6, parvovirus B19, Epstein-Barr virus, cytomegalovirus, Brucella, and Klebsiella—have all been investigated. A link to kinase mutations has been described in nodal and extranodal RDD; however, the molecular profile of cutaneous RDD remains unknown.2 Histologic findings for RDD typically include cells that are S100 positive, CD68 positive, and CD163 positive, and CD1a and langerin (CD207) negative, thus excluding Langerhans cell histiocytosis.2 The hallmark finding of RDD is emperipolesis, which results from “histiocyte-mediated phagocytosis of intact lymphocytes and other immune cells.”6 Immunoglobulin G (Ig) G4-positive plasma cells are also common, but the significance of this finding is controversial. We present a case of a patient with recurrent RDD within a right medial thigh lipoma and include a literature review to explore the significance of histologic findings and various treatment options in the setting of emerging treatment and diagnostic criteria.
Case Presentation
A 56-year-old African American male was evaluated in the rheumatology clinic at the Central Texas Veterans Affairs Medical Center in Temple, Texas, in 2022 for a cutaneous mass of his right medial thigh. The patient previously reported the onset of a right medial thigh mass in 2005 after he had been deployed in Iraq for about 1 year. A biopsy of the mass from 2005 showed infiltration of plasma cells, lymphocytes, and histiocytes and occasional neutrophils with noted reactivity of S100 protein and CD163, but not CD1a. The patient’s original biopsy report from March 2005 was obtained secondhand from an addendum to a Dermatology Consult note. Surgical excision of the mass was not performed until 2012 and systemic therapy was not initiated.
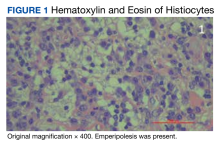
In 2021, the mass recurred and gradually increased in size, prompting a second surgical removal. Pathology results from the 2021 mass showed a lipoma with areas of fibrosis with a mixed inflammatory cell infiltrate, including abundant lymphocytes, plasma cells, occasional hemosiderin-laden histiocytes, and clusters of enlarged histiocytes with foamy to pale eosinophilic, finely granular cytoplasm, and large, round, vesicular nuclei with prominent nucleoli. Emperipolesis was also present (Figure 1).
Special immunohistochemical staining showed most of the lymphocytes were CD20 positive B-cells with a minority of CD3 positive T-cells. Histiocytes were CD163 positive and CD68 positive with patchy reactivity for S100 protein. The plasma cells were CD138 positive. There were > 125 IgG4-positive plasma cells present in a single high-powered field and the overall IgG4:IgG plasma cell ratio was > 40%. Pertinent imaging included a whole-body positron emission tomography/computed tomography (PET/CT) hypermetabolic activity scan of a small right femoral lymph node (9 mm) and nearby medial right femoral lymph node (13 mm) (Figure 2A). A well-defined mass in the medial aspect of the right thigh (2.5 cm x 3.2 cm x 3.9 cm) and a cutaneous/subcutaneous lesion of the anterior medial aspect of the proximal right thigh superior to the mass (2.9 cm) were also evident on imaging (Figure 2B). Each area of hypermetabolic activity had decreased in size and activity when compared to a previous PET/CT obtained 1 month earlier. There was no evidence of skeletal malignancy. A physical examination did not reveal any other soft tissue masses, palpable lymphadenopathy, or areas of skin involvement. Given the patient’s reassuring imaging findings and a lack of any new physical examination findings, no systemic therapy was initiated, and following shared decision making, the patient agreed to a period of watchful waiting.