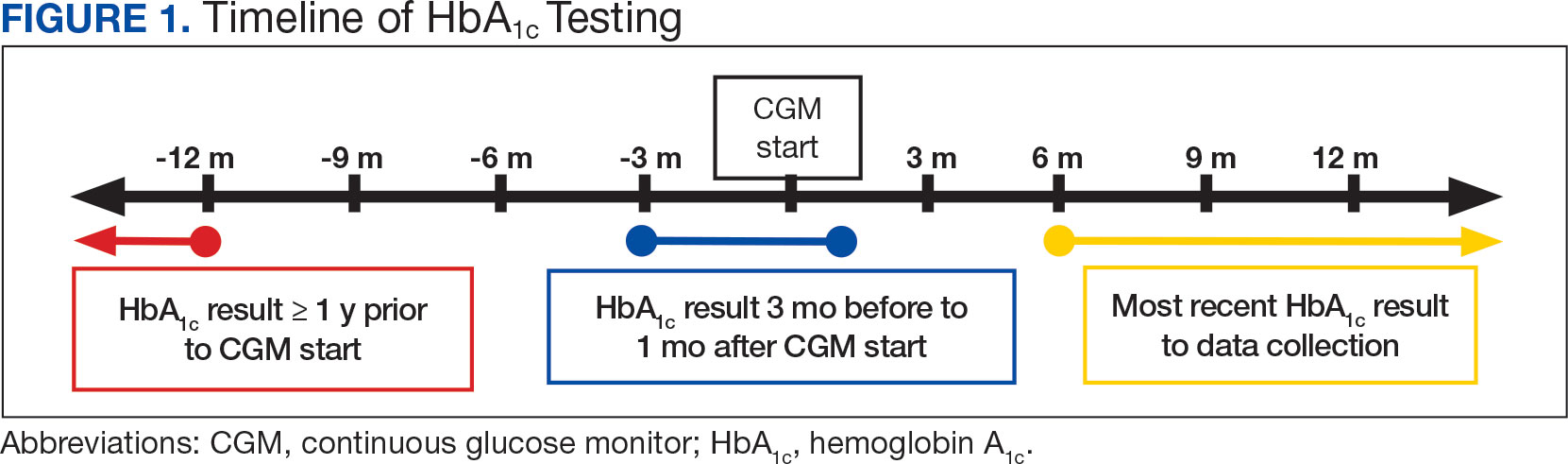
This study also explored secondary outcomes including changes in HbA 1c by prescriber type, differences in HbA 1c reduction based on age, and changes in diabetes medications, including total daily insulin doses. For secondary outcomes, diabetes medication information and the total daily dose of insulin were gathered at the start of CGM use and at the time of data collection. The most recent CGM order prescribed was also collected.
Veterans were included if they were aged ≥ 18 years, had an active order for a CGM, T2DM diagnosis, an insulin prescription, and previously used test strips for glucose monitoring. Patients with T1DM, those who accessed CGMs or care in the community, and patients without HbA 1c values pre-CGM, were excluded.
Statistical Analysis
The primary endpoint of change in HbA 1c level before and after CGM use was compared using a paired t test. A 0.5% change in HbA 1c was considered clinically significant, as suggested in other studies. 8,9 P < .05 was considered statistically significant. Analysis for continuous baseline characteristics, including age and total daily insulin, were reported as mean values. Nominal characteristics including sex, race, diabetes medications, and prescriber type are reported as percentages.
Results
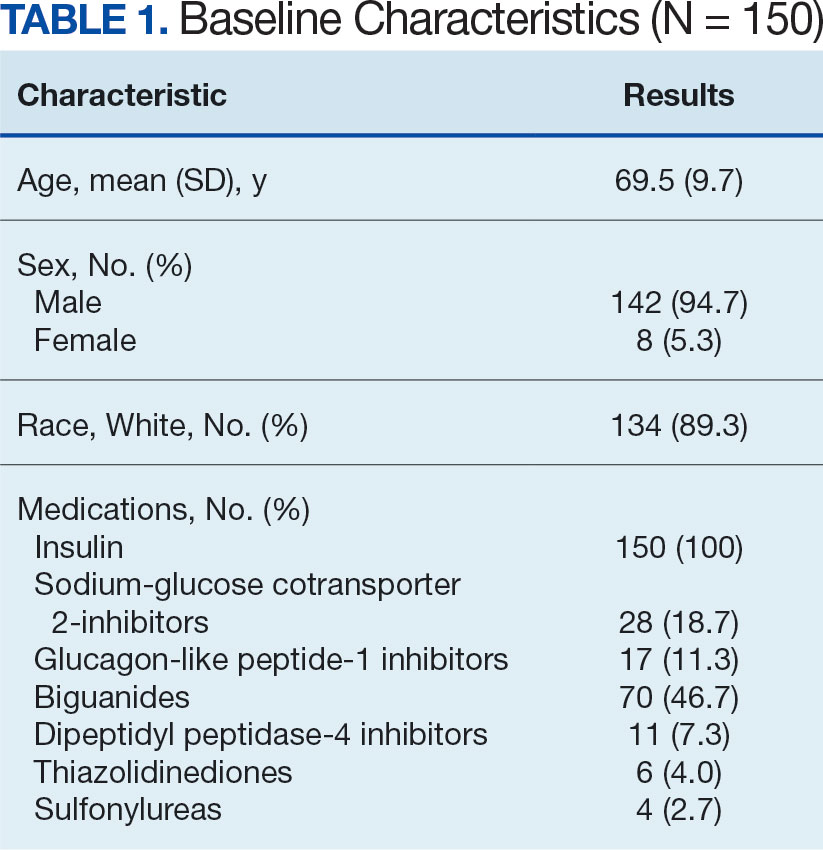
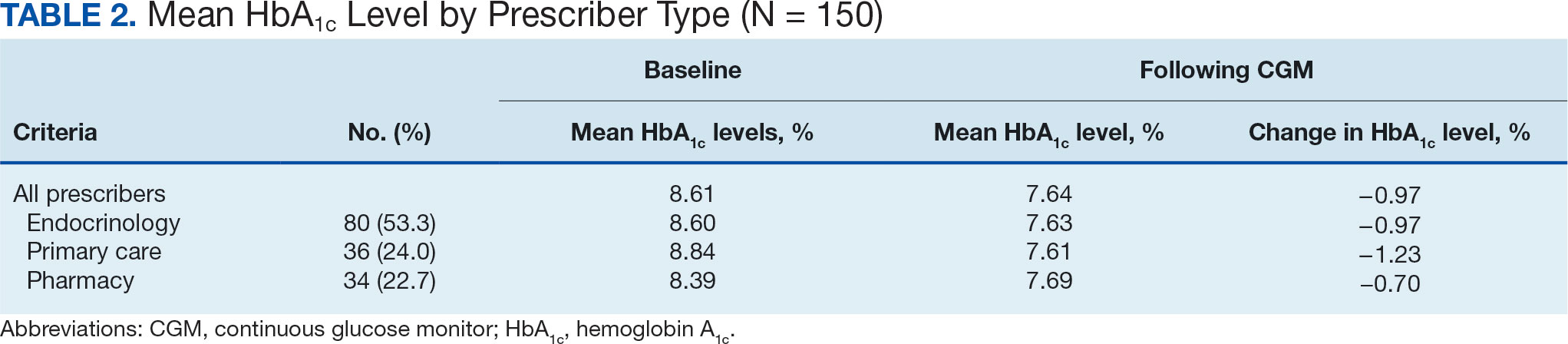
A total of 402 veterans were identified with an active CGM at the time of initial data collection in January 2024 and 175 met inclusion criteria. Sixty patients were excluded due to diabetes managed through a community HCP, 38 had T1DM, and 129 lacked HbA 1c within all specified time periods. The 175 veterans were randomized, and 150 were selected to perform a chart review for data collection. The mean age was 70 years, most were male and identified as White (Table 1). The majority of patients were managed by endocrinology (53.3%), followed by primary care (24.0%), and pharmacy (22.7%) (Table 2). The mean baseline HbA 1c was 8.6%.
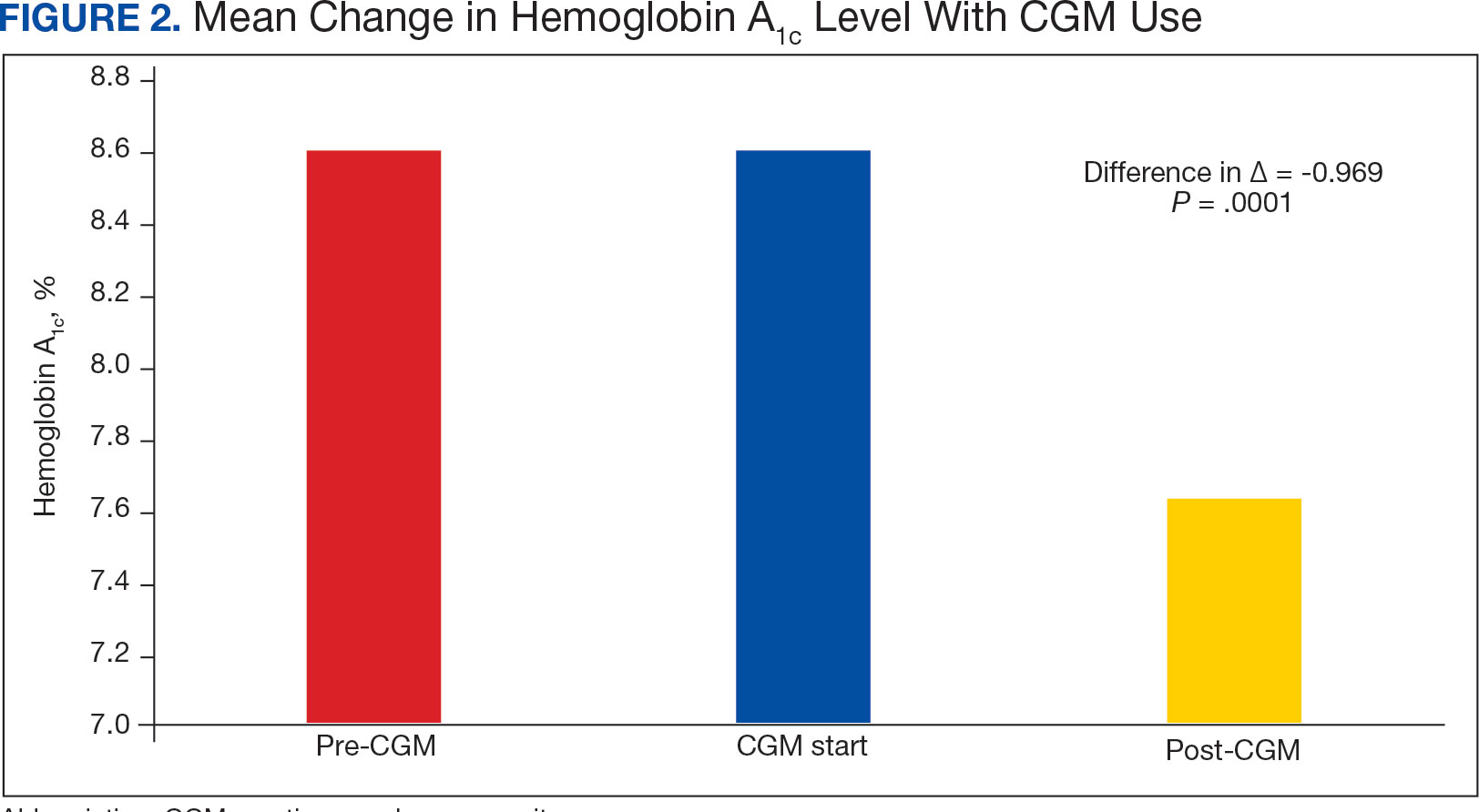
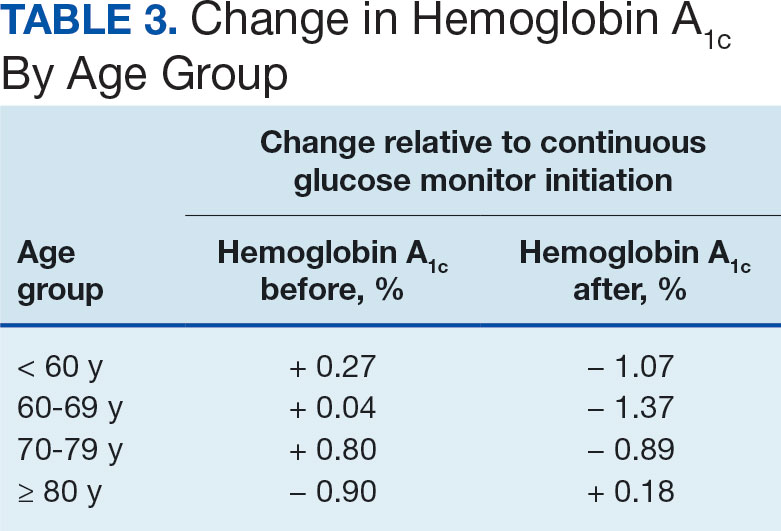
The difference in HbA 1c before and after use of CGM was -0.97% ( P = .0001). Prior to use of a CGM the change in HbA 1c was minimal, with an increase of 0.003% with the use of selfmonitoring glucose. After use of a CGM, HbA 1c decreased by 0.971%. This reduction in HbA 1c would also be considered clinically significant as the change was > 0.5%. The mean pre-, at start, and post-CGM HbA 1c levels were 8.6%, 8.6%, and 7.6%, respectively (Figure 2). Pharmacy prescribers had a 0.7% reduction in HbA 1c post-CGM, the least of all prescribers. While most age groups saw a reduction in HbA 1c, those aged ≥ 80 years had an increase of 0.18% (Table 3). There was an overall mean reduction in insulin of 22 units, which was similar between all prescribers.
Discussion
The primary endpoint of difference in change of HbA 1c before and after CGM use was found to be statistically and clinically significant, with a nearly 1% reduction in HbA 1c, which was similar to the reduction found by Vigersky and colleagues. 5 Across all prescribers, post-CGM HbA 1c levels were similar; however, patients with CGM prescribed by pharmacists had the smallest change in HbA 1c. VA pharmacists primarily assess veterans taking insulin who have HbA 1c levels that are below the goal with the aim of decreasing insulin to reduce the risk of hypoglycemia, which could result in increased HbA1c levels. This may also explain the observed increase in post-CGM HbA 1c levels in patients aged ≥ 80 years. Patients under the care of pharmacists also had baseline mean HbA1c levels that were lower than primary care and endocrinology prescribers and were closer to their HbA 1c goal at baseline, which likely was reflected in the smaller reduction in post-CGM HbA 1c level.