Design and Referral
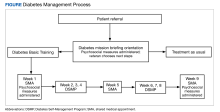
Self-management programs for chronic health conditions are often underutilized. Although HCPs may wish to connect veterans with available programs, time constraints may limit opportunities for detailed discussions with patients about specific aspects of each program. To simplify this process, a 2-hour orientation program was offered that explained individual and group DM self-management options (Figure). During this initial visit, patients met with an interdisciplinary care team (registered dietician, diabetes nurse practitioner, and behavioral health specialist) and were informed about Diabetes Basic Training, DM clinical care practices, and other related resources available at the Cincinnati VAMC (eg, cooking classes, food pantry). Patients received individualized referral recommendations and were urged to consult with their primary care practitioner to finalize their treatment plan.
Shared Medical Appointments
Diabetes Basic Training interventions had an average of 6 to 8 veterans participating in the weekly groups. The first, fifth, and final weeks were SMAs in which an interdisciplinary team collaboratively provided group-based health care for DM. The team consisted of a registered nurse, a prescriber (eg, nurse practitioner), a moderator (eg, psychologist), and a content expert (eg, nutritionist). Before each SMA began, the nurse checked-in patients in the SMA room and collected heart rate and blood pressure, and performed a diabetic foot check. Each SMA consisted of introductions, group-driven discussions (facilitated by an HCP) and troubleshooting DM self-management challenges. During group discussions, the prescriber initiated a 1-on-1 discussion with each patient in a private office regarding their recent laboratory results, medication regimen, and other aspects of DM care. The patient’s medications were refilled and/or adjusted as needed and other orders and referrals were submitted. If a patient had a medical question, the prescriber and moderator engaged the entire group so all individuals could benefit from generating and hearing answers. When discussion slowed, education was provided on topics generated by the group. Frequent topics included challenges managing DM, concerns, how DM impacted daily life and relationships, and sharing successes. As needed, HCPs spoke individually with patients following the SMA. Patients were sometimes asked, but never required, to do homework consistent with standard DM care (eg, recording what they eat or blood sugar levels). Each SMA session lasted about 2 hours.
Diabetes Self-Management Program
The second, third, fourth, sixth, seventh, and eighth weeks of the program were devoted to the DSMP. These sessions were delivered primarily by veteran peers who received appropriate training, observation, and certification. Each 2-hour educational program provided ample practice in many fundamental self-management skills, such as decision making, problem solving, and action planning. Patients were asked, but never required, to practice related skills during the sessions and to create weekly action plans to be completed between sessions that typically involved increasing exercise or improving diet. Patients were encouraged to follow up with HCPs at SMAs when they had questions requiring HCP expertise. If participants had more immediate concerns regarding their treatment plan and/or medications, they contacted their primary care practitioner prior to the next SMA.
As a part of participation in the program, psychosocial and health data and Hb A1c levels at baseline (the closest level to 90 days prior to start) and follow-up (the closest level to 90 days after the final session) were collected.8 In addition, Problem Areas in Diabetes (PAID), Patient Activation Measure (PAM)-13, and Diabetes Self-Management Questionnaire (DSMQ) were administered at 3 points: during the orientation, in the first week, and in the ninth week of the program.
PAID, a 20-item self-report questionnaire designed to capture emotional distress related to having DM, is a valid and reliable scale able to detect changes over time when used in intervention studies.9,10 PAM-13 is a 13-item measure designed to assess patient knowledge, skill, and confidence in the self-management of health or chronic conditions based on the original PAM.11,12 Scores fall into 1 of 4 activation levels, ranging from low levels of confidence and knowledge of health management to high levels of being proactive with one’s care. The PAM-13 has been widely used within health psychology, including research among adults with multiple chronic conditions, individuals with DM or osteoarthritis, and within primary care.13-15 The DSMQ is a statistically reliable and valid instrument that allows for user-friendly assessment of self-care behaviors associated with glycemic control.16-18