Implementation
EHJVAH is a 1A facility with > 80 patients who receive outpatient hemodialysis on campus. At the time of this collaboration in the fall of 2019, the collaborative dialysis team comprised 2 social workers and a nephrologist. The PC team included a coordinator, 2 nurse practitioners, and 3 physicians. A QI nurse was involved in the initial data gathering for this project.
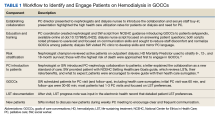
The PC and nephrology medical directors developed a workflow process that reflected organizational and clinical steps in planning, initiating, and completing GOCCs with patients on outpatient dialysis (Table 1). The proposed process engaged an interdisciplinary PC and nephrology group and was revised to incorporate staff suggestions.
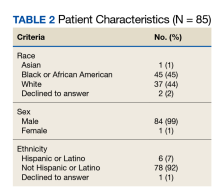
A prospective review of 85 EHJVAH hemodialysis unit patient records was conducted between September 1, 2019, and September 30, 2020 (Table 2). We reviewed LST completion rates for all patients receiving dialysis within this timeframe. During the intervention period, the PC team approached 40 patients without LST notes to engage in GOCCs. PC completed LST notes for 29 of 40 patients (72%). Of the 11 patients without LST notes, 7 declined a visit and 4 were lost to follow-up. At the end of the study period, 69 patients (81%) on outpatient dialysis had LST progress notes in the EHR.
Discussion
Over the 13-month collaboration, LST note completion rates increased from 27% to 81%, with 69 of 85 patients having a documented LST progress note in the EHR. PC approached nearly half of all patients on dialysis. Most patients agreed to be seen by the PC team, with 72% of those approached agreeing to a PC consultation. Previous research has suggested that having a trusted dialysis staff member included in GOCCs contributes to high acceptance rates.12 As such, the QI project relied heavily on the existing rapport between the dialysis staff—in particular the dialysis social workers—and their patients to normalize the PC consultation for all patients on dialysis. This introduction by a trusted staff person may have contributed to higher acceptance rates, and at the time patients on dialysis arrived for the PC appointment, they had a good understanding of the project. By including PC specialists with expertise in advance care planning and communication skills, the partnership successfully created a collaborative process that relied on the skill set of multiple staff and disciplines.
PC is a relatively uncommon partnership for nephrologists, and PC and hospice services are underutilized in patients on dialysis both nationally and within the VA.13-15 Our outcomes could be replicated, as PC is required at all VA sites. One implementation consideration is the additional time this collaboration requires. Although no formal time study was completed, the PC team spent several hours educating nephrology staff, and the social workers spent considerable time reaching, educating, and scheduling veterans into the PC clinic.
Conclusions
The innovation of an interdisciplinary nephrology–PC collaboration was an important step in increasing high-quality GOCCs and eliciting patient preferences for LSTs among patients on dialysis. PC integration for patients on dialysis is associated with improved symptom management, fewer aggressive health care measures, and a higher likelihood of dying in one’s preferred setting.16 While this partnership focused on patients already receiving dialysis, successful PC interventions are felt most keenly upstream, before dialysis initiation.
Acknowledgments
The authors acknowledge the contributions of their colleague, Mary McCabe, DNP, Quality Systems Improvement, Edward Hines, Jr. Veterans Affairs Hospital. The authors also acknowledge the clinical dedication of the dialysis social workers, Sarah Adam, LCSW, and Sarah Kraner, LCSW, without which this collaboration would not have been possible.