HOT-CRT: Randomized CSP vs. BiV pacing trial
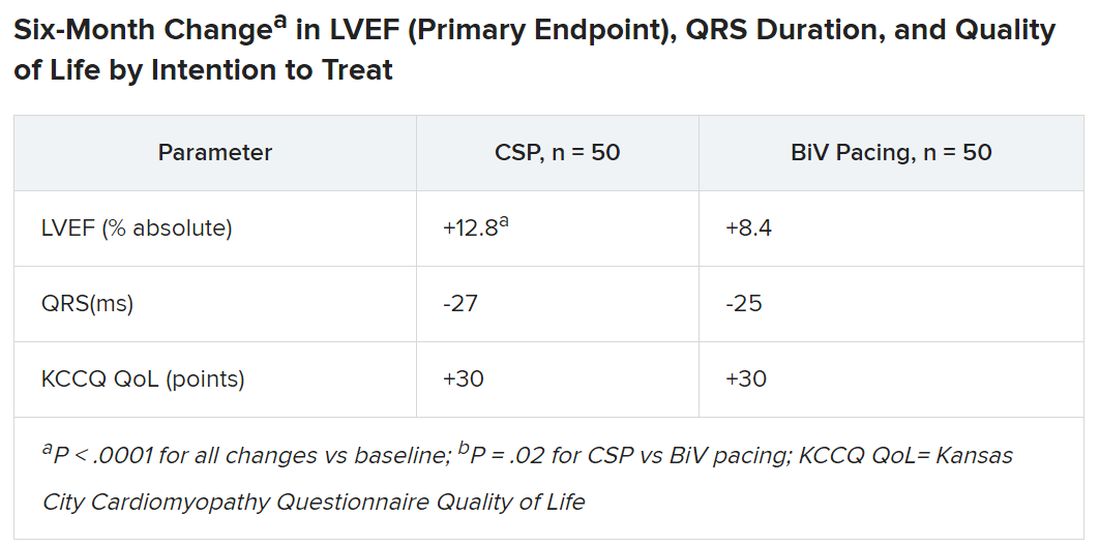
Conducted at three centers in a single health system, the His-optimized cardiac resynchronization therapy study (HOT-CRT) randomly assigned 100 patients with primary or secondary CRT indications to either to CSP – by either His-bundle or LBB-area pacing – or to standard BiV-CRT as the first-line resynchronization method.
Treatment crossovers, allowed for either pacing modality in the event of implantation failure, occurred in two patients and nine patients initially assigned to CSP and BiV pacing, respectively (4% vs. 18%), Dr. Vijayaraman reported.
Historically in trials, BiV pacing has elevated LVEF by about 7%, he said. The mean 12-point increase observed with CSP “is huge, in that sense.” HOT-CRT enrolled a predominantly male and White population at centers highly experienced in both CSP and BiV pacing, limiting its broad relevance to practice, as pointed out by both Dr. Vijayaraman and his presentation’s invited discussant, Yong-Mei Cha, MD, Mayo Clinic, Rochester, Minn. Dr. Cha, who is director of cardiac device services at her center, also highlighted the greater rate of crossover from BiV pacing to CSP, 18% vs. 4% in the other direction. “This is a very encouraging result,” because the implant-failure rate for LBB-area pacing may drop once more operators become “familiar and skilled with conduction-system pacing.” Overall, the study supports CSP as “a very good alternative for heart failure patients when BiV pacing fails.”
International comparison of CSP and BiV pacing
In Dr. Vijayaraman’s other study, the observational comparison of LBB-area pacing and BiV-CRT, the CSP technique emerged as a “reasonable alternative to biventricular pacing, not only for improvement in LV function but also to reduce adverse clinical outcomes.”
Indeed, in the international study of 1,778 mostly male patients with primary or secondary CRT indications who received LBB-area or BiV pacing (797 and 981 patients, respectively), those on CSP saw a significant drop in risk for the primary endpoint, death or HFH.
Mean LVEF improved from 27% to 41% in the LBB-area pacing group and 27% to 37% with BiV pacing (P < .001 for both changes) over a follow-up averaging 33 months. The difference in improvement between CSP and BiV pacing was significant at P < .001.
In adjusted analysis, the risk for death or HFH was greater for BiV-pacing patients, a difference driven by HFH events.
- Death or HF: hazard ratio, 1.49 (95% confidence interval, 1.21-1.84; P < .001).
- Death: HR, 1.14 (95% CI, 0.88-1.48; P = .313).
- HFH: HR, 1.49 (95% CI, 1.16-1.92; P = .002)
The analysis has all the “inherent biases” of an observational study. The risk for patient-selection bias, however, was somewhat mitigated by consistent practice patterns at participating centers, Dr. Vijayaraman told this news organization.
For example, he said, operators at six of the institutions were most likely to use CSP as the first-line approach, and the same number of centers usually went with BiV pacing.