Step 3: proposal
There are no standardized formats for presenting a VHA business proposal; however, this outline provides a template. The business proposal should be designed to effectively communicate the collective data that describe the needs and requirements of a PD program to the local, regional, and national leadership. Not every rationale presented here will apply to an individual proposal and the local champion will need to tailor their rationale for their locale. A sample business plan is shown in eAppendix 3 (available online at doi:10.12788/fp.0356). VHA Handbook of dialysis requires that a PD nurse has a minimum of 12 months of nursing experience with at least 3 months of PD experience.25 Nursing training, education, and support should be discussed with nursing leadership and included in the business plan. Similarly, arrangements for laboratory, pharmacy, and prosthetics services and/or logistics to facilitate procurement of the needed devices, disposables, and supplies are essential and should be highlighted in the business plan.
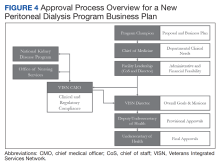
Approval Process
Though the initial explorations are conventionally undertaken with the support of the local leadership, starting a PD program is considered an augmentation of clinical services and thus requires multistage VHA approvals (Figure 4). The business proposal progresses through the local medicine service leadership and chief of staff to the facility director. The rationale presented in this review is general and has been drawn from the collective experience of authors and under the guidance of the VHA NKDP. However, it still requires deliberation by the local leadership, comprised of nonnephrology clinicians and administrative professionals to ensure its soundness and sustainability. Once approved locally, the VISN chief medical officer aided by the opinions from the NKDP office conducts a thorough evaluation of infrastructure allocations, supplies and support services, skills, competencies, and the privileges of all clinical and ancillary staff, and may conduct a site visit by an expert panel through the responsible clinical program office. The VISN director may also request changes to match any local mandates before approvals. Once approved, the VISN office simultaneously forwards the proposal to several services, including the Office of Nursing Services and the Office of Patient Care Services, which reviews the proposal for the appropriateness and determines the need for an on-site review before approval. These composite reviews and recommendations guide the highest offices in finalizing the decision, with the final approvals from the Under Secretary for Health.Postapproval Process
Once approved, the champion will need to work closely with various services and managers to oversee infrastructural renovations and execute the hiring plans, establish standard operating procedures (SOPs), standardize staff proficiencies and functional statements, and finalize quality assessment parameters. Home dialysis standards have been addressed by NKDP and The Joint Commission. While PD requires home visits to assess the appropriateness of the environment, the PD program is accredited under hospital-based therapy. Standards and performance metrics should be incorporated into all the VA PD programs for standardization and assessment. Based on guidance from the VHA Handbook, quality metrics, such as dialysis adequacy, and rates of infection should be monitored and reviewed. The dialysis director may need to consider more frequent program evaluations in the first year to ensure appropriate troubleshooting. The VA infrastructure has developed the resources for a central repository for the PD SOPs and quality metrics, which can be obtained and adapted for the local program. Similarly, veteran satisfaction can be assessed through existing resources. Finally, the dialysis director can join the National VHA Dialysis Director listserv for regular updates on the existing and new VHA policies and NKDP updates.
Conclusions
Establishing a new PD program within a local federal infrastructure can appear daunting, both in terms of planning as well as approvals. However, the provision of home-based dialysis therapies may be beneficial to those in rural settings with limited access to in-center dialysis modalities as well as to those who seek autonomy and lifestyle independence in their medical care. Collaborations with the VHA NKDP or PD workgroup can help overcome many of the procedural hurdles, provide guidance about infrastructure and resource allocation and utilization, and provide easy access to established SOPs and quality parameters.
Acknowledgments
We acknowledge the late Dr. Catherine Do for her significant contribution to this manuscript. We also extend our sincere thanks to Dr. Holly Mattix-Kramer (Edward Hines Jr. Veterans Affairs Hospital and Loyola University Medical Center) for her prompt and valuable feedback on this manuscript.