AHOBPR Overview
The AHOBPR is an online questionnaire and optional in-person health evaluation that includes 7 major categories targeting deployment history, symptoms, medical history, health concerns, residential history, nonmilitary occupational history, nonmilitary environmental exposures, and health care utilization. The VA Defense Information Repository is used to obtain service dates for the service member/veteran, conflict involvement, and primary location during deployment. The questionnaire portion of the AHOBPR is administered online. It currently is open to all veterans who served in the Southwest Asia theater of operations (including Iraq, Kuwait, and Egypt) any time after August 2, 1990, or Afghanistan, Djibouti, Syria, or Uzbekistan after September 11, 2001. Veterans are eligible for completing the AHOBPR and optional health evaluation at no cost to the veteran regardless of VA benefits or whether they are currently enrolled in VA health care. Though the focus of the present manuscript is to profile a VA program, it is important to note that the US Department of Defense (DoD) is an active partner with the VA in the promotion of the AHOBPR to service members and similarly provides health evaluations for active-duty service members (including activating Reserve and Guard) through their local MTF.
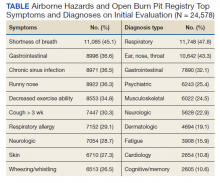
We reviewed and analyzed AHOBPR operations and VA data from 2014 to 2020. Our analyses were limited to veterans seeking evaluation as well as their corresponding symptoms and HCP’s clinical impression from the electronic health record. As of September 20, 2021, 267,125 individuals completed the AHOBPR. The mean age was 43 years (range, 19-84), and the majority were male (86%) and served in the Army (58%). Open-air burn pits (91%), engine maintenance (38.8%), and convoy operations (71.7%) were the most common deployment-related exposures.
The optional in-person AHOBPR health evaluation may be requested by the veteran after completing the online questionnaire and is performed at the veteran’s local VA facility. The evaluation is most often completed by an environmental health clinician or primary care practitioner (PCP). A variety of resources are available to providers for training on this topic, including fact sheets, webinars, monthly calls, conferences, and accredited e-learning.20 As part of the clinical evaluation, the veteran’s chief concerns are assessed and evaluated. At the time of our analysis, 24,578 clinical examinations were performed across 126 VA medical facilities, with considerable geographic variation. Veterans receiving evaluations were predominantly male (89%) with a median age of 46.0 years (IQR, 15). Veterans’ major respiratory concerns included dyspnea (45.1%), decreased exercise ability (34.8%), and cough > 3 weeks (30.3%) (Table). After clinical evaluation by a VA or MTF HCP, 47.8% were found to have a respiratory diagnosis, including asthma (30.1%), COPD (12.8%), and bronchitis (11.9%).
Registry participants who opt to receive the clinical evaluation may benefit directly by undergoing a detailed clinical history and physical examination as well as having the opportunity to document their health concerns. For some, clinicians may need to refer veterans for additional specialty testing beyond this standard AHOBPR clinical evaluation. Although these evaluations can help address some of the veterans’ concerns, a substantial number may have unexplained respiratory symptoms that warrant further investigation.
Post-Deployment Cardiopulmonary Evaluation Network Clinical Evaluation
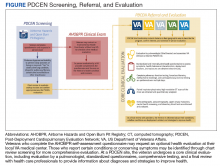
In May 2019, the VA established the Airborne Hazards and Burn Pits Center of Excellence (AHBPCE). One of the AHBPCE’s objectives is to deliver specialized care and consultation for veterans with concerns about their postdeployment health, including, but not limited to, unexplained dyspnea. To meet this objective, the AHBPCE developed the PDCEN, a national network consisting of specialty HCPs from 5 VA medical centers—located in San Francisco, California; Denver, Colorado; Baltimore, Maryland; Ann Arbor, Michigan; and East Orange, New Jersey. Collectively, the PDCEN has developed a standardized approach for the comprehensive clinical evaluation of unexplained dyspnea that is implemented uniformly across sites. Staff at the PDCEN screen the AHOBPR to identify veterans with features of respiratory disease and invite them to participate in an in-person evaluation at the nearest PDCEN site. Given the specialty expertise (detailed below) within the Network, the PDCEN focuses on complex cases that are resource intensive. To address complex cases of unexplained dyspnea, the PDCEN has developed a core clinical evaluation approach (Figure).
The first step in a veteran’s PDCEN evaluation entails a set of detailed questionnaires that request information about the veteran’s current respiratory, sleep, and mental health symptoms and any associated medical diagnoses. Questionnaires also identify potential exposures to military burn pits, sulfur mine and oil field fires, diesel exhaust fumes, dust storms, urban pollution, explosions/blasts, and chemical weapons. In addition, the questionnaires include deployment geographic location, which may inform future estimates of particulate matter exposure.21 Prior VA and non-VA evaluations and testing of their respiratory concerns are obtained for review. Exposure and health records from the DoD are also reviewed when available.
The next step in the PDCEN evaluation comprises comprehensive testing, including complete pulmonary function testing, methacholine challenge, cardiopulmonary exercise testing, forced oscillometry and exhaled nitric oxide testing, paired high-resolution inspiratory and expiratory chest computed tomography (CT) imaging, sinus CT imaging, direct flexible laryngoscopy, echocardiography, polysomnography, and laboratory blood testing. The testing process is managed by local site coordinators and varies by institution based on availability of each testing modality and subspecialist appointments.
Once testing is completed, the veteran is evaluated by a team of HCPs, including physicians from the disciplines of pulmonary medicine, environmental and occupational health, sleep medicine, otolaryngology and speech pathology, and mental health (when appropriate). After the clinical evaluation has been completed, this team of expert HCPs at each site convenes to provide a final summary review visit intended to be a comprehensive assessment of the veteran’s primary health concerns. The 3 primary objectives of this final review are to inform the veteran of (1) what respiratory and related conditions they have; (2) whether the conditions is/are deployment related; and (3) what treatments and/or follow-up care may enhance their current state of health in partnership with their local HCPs. The PDCEN does not provide ongoing management of any conditions identified during the veteran’s evaluation but communicates findings and recommendations to the veteran and their PCP for long-term care.