It is currently unknown how many veterans follow through with these instructions. Nonetheless, if veterans are deemed eligible, they may present to VHA to obtain a same-day appointment. If not eligible, a suicide prevention coordinator may give them the phone number of a community referral. However, this practice is not standardized across VA medical centers, and the provided resources are up to the suicide prevention coordinator to research. Additionally, when a VHA suicide prevention coordinator leaves the position, knowledge of these community resources and rapport with community HCPs are often lost, leaving the next coordinator to develop these again, which reduces the efficiency and effectiveness of limited resources. It is also unknown how many veterans complete this contact and receive evidence-based treatment following referral. This is a complex system to navigate, particularly when at risk for suicide and in need of immediate but not emergency services.
Suicide prevention in such circumstances may be improved by adapting current suicide prevention practices, including evidence-based interventions, and the new VHA intensive case management program,11,36 within a Zero Suicide framework. PSCI-SPC has developed a brief intervention to transition ineligible veterans to permanent community treatment and provide them with additional resources to meet their varied needs. The brief 1 to 3 session intervention combines practices from brief cognitive behavioral therapy (BCBT) for suicide prevention, crisis response planning (CRP), and intensive case management within a Zero Suicide framework. Both the 2019 VA/DoD suicide prevention clinical practice guidelines and Zero Suicide recommend using cognitive behavioral therapy (CBT)-based interventions for suicide prevention.11,32 These interventions are packaged into a single intervention delivered by a PSCI-SPC therapist, typically a licensed clinical social worker, a licensed clinical psychologist, or an unlicensed psychologist under the supervision of a licensed clinical psychologist.
BCBT is one type of CBT that has shown initial efficacy in reducing suicide attempts.37 BCBT reduces the risk for suicide attempts both at the conclusion of treatment and at 24-month follow-up.37 BCBT is boiled down to its most essential components so it can be delivered in a distilled format. An essential element of BCBT that will remain is the CRP. A CRP11,37,38 entails collaboratively identifying effective, appropriate coping strategies and specific individuals to contact during a crisis. CRPs demonstrated efficacy as a stand-alone intervention to existing suicide prevention methods in a randomized clinical trial, such that individuals who received CRP had faster reductions in suicidal ideation and were 76% less likely to make a suicide attempt during the 6-month follow-up period.39 These results demonstrate that use of a CRP is connected to a decrease in suicidal behavior among suicidal patients.
The VHA has developed and is piloting a new initiative focused on restructuring its intensive case management services. RACETIME to Integrated Care (eg, Risk stratification, Assessment of complexity, Coordinator of lead assignment, Evaluate whole health needs, Trusting partnerships, Integrate care, Monitor progress, Experience of the veteran and employee) is a framework that assists VHA case managers in transitioning from a traditional case management mind-set to a more integrated and holistic method of care.36 RACETIME intensive case management practices will be incorporated into the intervention. However, RACETIME focuses on case management internally to the VHA. A modification for this treatment will be to focus on intensive case management from a mental health perspective and connecting to external community resources. Community referrals are mapped within a structured process and stored on a shared drive. This improves continuity between suicide prevention coordinators when they leave for a new position.
This intervention is conducted within a Zero Suicide framework. Pertinent to PSCI-SPC innovation to enhance care for non-VHA veterans is the care transitions element within the Zero Suicide framework, which has developed comprehensive suicide prevention guidance, including a pathway to care.32 This pathway refers a process to conduct follow-up supportive contacts that are tracked and recorded.
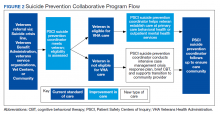
The PSCI-SPC pilot program incorporates the elements of CRP and brief CBT within a Zero Suicide framework. The PSCI-SPC team is developing and testing a protocol for providing brief treatment and community referrals to ineligible veterans that integrates these programming elements (Figure 2). A PSCI-SPC social worker will coordinate with the eligibility office to determine VHA eligibility. Ineligible veterans are referred to community partners and nonenrolled, eligible veterans are linked to VHA HCPs if they desire. These transitions will be coordinated, closely monitored, and verified. The PSCI-SPC team receives referrals from the VCL and other VHA programs that are in contact with ineligible veterans. Other program eligibility criteria include meeting 1 of 3 criteria: (1) a lifetime suicide attempt; (2) suicidal ideation in the past 6 months; or (3) a current mental health disorder. At the outset of the program, it is explained that the purpose of the intervention is to provide short-term, transitional services to assist the veteran in attaining a permanent mental health placement.
Once the eligibility is determined, and the veteran’s preference is assessed, the team will perform a warm handoff to a VHA representative for enrollment into VHA care or to a community placement. We have sourced multiple community placements at varied payor levels. All veterans who are ineligible for care or who do not desire to be enrolled in VHA care will be provided the intervention package described above. After the veteran is placed in community care, PSCI-SPC team will follow up regularly with the veteran for 3 months to ensure continuity of care. If additional sessions are needed while the veteran needs a community placement, the PSCI team can accommodate this and will track the number of participants who needed additional sessions. If the veteran is deemed to be at imminent risk for suicide at any time during the pilot, he/she is transferred to emergency care. The veteran is allowed to participate once stabilized.
Findings from the pilot program will inform a manual intended for dissemination to patient safety and suicide prevention coordinators nationally across the VHA. The products from this objective will be integrated with the other objectives in training that will be provided on how to develop a local collaborative (Objective 1), disseminate the toolkit (Objective 2), and receive referrals into VHA or refer veterans to community clinical partners through the pilot program (Objective 3). Products developed and disseminated throughout PSCI-SPC aim to create momentum to reduce rates of suicide in veterans who are not connected to the VHA at the local community level.