Translating System Changes Into Better Care
Despite transformative changes to Army behavioral health care, clinicians and leaders still had little insight into what mattered most: measuirng patient response to the treatment. To solve this issue, a team of Army clinical and information technology innovators developed the Behavioral Health Data Portal (BHDP), which used validated scales to collect input from patients at each outpatient visit about their current and recent symptoms. Clinicians use the information to complement their assessment, refine diagnoses, individualize treatment plans, and follow their patients’ progress.9
The BHDP also aggregates information on each patient’s progress into clinical outcome metrics that inform leaders about the effectiveness of the care their clinics provide. For the first time, analysts can establish correlations between specific actions at the clinic level and positive clinical outcomes. For example, the relationship between the use of evidence-based psychotherapies, regular follow-up, a strong therapeutic alliance, and provider use of BHDP have been clearly linked to more rapid resolution of PTSD symptoms. These insights provide opportunities to act on specific processes at the clinic level with high confidence that by doing so, clinicians are improving the effectiveness of the care delivered in their clinics.
Conclusion
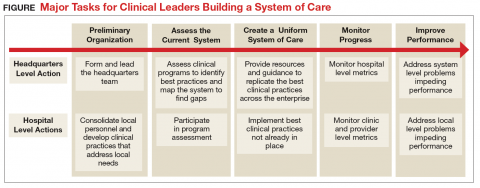
The transformation of Army behavioral health care has encompassed all aspects of the treatment system, but it has been led by clinicians working at the local and headquarters levels (Figure). Although many challenges remain, today’s outpatient system is more efficient and effective. For example, Army medical facilities are now able to meet more of the total demand for outpatient behavioral health care of its beneficiaries; 77% in September 2017 compared with a low of 59% in January 2013, based on Army Strategic Management System data as of December 1, 2017. With a better organized outpatient system, clinicians have less frequently relied on costly and stigmatizing inpatient care. Soldiers required 40% fewer inpatient bed days in 2016 than they did in 2012, based on Military Health System Management and Reporting Tool (M2) data as of July 1, 2017.
The Army continues to improve its system of care to better inform and enable clinicians to deliver evidence-based care. The clinician-led process that advanced this area of military medicine is applicable to others. A core group of dedicated clinical professionals committed to multiyear processes can implement large-scale changes if they are empowered and resourced by senior medical leaders. A standardized system of care built on clinical best practices and guided by clinicians using accurate data, including clinical outcomes, would benefit any component of the MHS.