Results
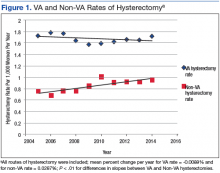
A retrospective query of the CDW identified 8,327 hysterectomies performed at the VA for benign indications from fiscal year (FY) 2005 to FY 2014. The total number of annual hysterectomies at the VA increased 30.7% from 710 in FY 2004 to 1,025 in FY 2014. The annual number of women veterans who accessed VA health care increased 30.8% from 412,271 to 596,011 during the same time frame. Thus, the population adjusted hysterectomy rate remained stable at 1.72 (Figure 1).
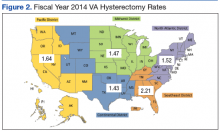
The table shows the relative proportion of hysterectomy cases performed at the VA by age, indication for surgery, and geographic location stratified by route of hysterectomy. The mean age at time of hysterectomy was 44.2 (SD 7.7) years. The most frequent indications for all types of hysterectomy were uterine leiomyoma (41.4%), abnormal bleeding (25.3%), pelvic pain (14.0%), and pelvic organ prolapse (5.6%) (Table). Because of this study’s large sample size, there were significant differences among the hysterectomy types when comparing age, surgical diagnosis, and district.The authors also analyzed the VA data by district and decided to highlight the most recent data trends, as this is most applicable to how the VA currently operates. During FY 2014, the VA hysterectomy rates were as follows: district 1 (North Atlantic) 1.52; district 2 (Southeast) 2.21; district 3 (Midwest) 1.47; district 4 (Continental) 1.43; and district 5 (Pacific) 1.64 (Figure 2)
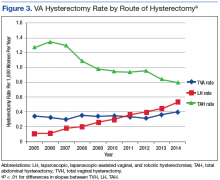
. District 2 had the highest adjusted hysterectomy rate, and district 3 had the highest percentage of minimally invasive hysterectomies (63.8%).During the study period, calculated hysterectomy rates based on route at the VA showed that the laparoscopic hysterectomy rate increased from 0.11 to 0.53, the vaginal hysterectomy rate remained relatively stable at 0.34 to 0.37, and the abdominal hysterectomy rate declined from 1.28 to 0.8 (Figure 3).
The percentage of hysterectomies performed via a minimally invasive approach increased from 25.9% (184/710) to 53.7% (550/1,025), (RR 2.1; 95% CI 1.9, 2.4). More specifically the percentage of laparoscopic hysterectomy increased from 6.2% (44/710) to 30.6% (314/1,025), (RR 5.7; 95% CI 4.5, 7.0; P < .0001), vaginal hysterectomy increased from 19.7% (140/710) to 23% (236/1,025), (RR 1.7; 95% CI 1.4, 2.0; P < .0001), and abdominal hysterectomy declined from 74.1% (526/710) to 46.3% (475/1,025), (RR 0.48; 95% CI 0.4, 0.5; P < .0001). From the Non-VA Care Cube, 4,296 women veterans were identified who underwent hysterectomy for benign indications at referral non-VA facilities from FY 2005 to FY 2014. The total number of patients referred annually to non-VA facilities for hysterectomy increased 45% from 312 to 567, with an increase in the population adjusted hysterectomy rate from 0.76 to 0.95 (Figure 1).Discussion
Although the total hysterectomy rate within the VA remained stable during the study period, the minimally invasive hysterectomy rate increased significantly. In FY 2014, the majority of hysterectomies at the VA were performed via a minimally invasive approach. Minimally invasive hysterectomy has many recognized advantages over abdominal hysterectomy as it offers a significant reduction in postoperative pain, narcotic use, length of stay, intraoperative blood loss, fever, deep venous thrombosis, and a faster recovery with return to baseline functioning thus improving overall quality of life.5-7 Previous literature of VA hysterectomy data from 1991 to 1997 reported an abdominal hysterectomy percentage of 74%, vaginal hysterectomy percentage of 22%, and laparoscopic assisted vaginal hysterectomy percentage of 4%.8
Additionally, previous literature of the civilian sector reported a national laparoscopic hysterectomy percentage of 32.4% in 2012, which is comparable to the laparoscopic hysterectomy percentage found in this study.9,10 These data highlight the growth of laparoscopic hysterectomy at the VA, which is comparable to that of the civilian sector.The Nationwide Inpatient Sample reported an abdominal hysterectomy percentage of 66.1% in 2003 and 52.8% in 2012.9,10 The authors observed a similar decline in the abdominal hysterectomy rate at the VA over the period studied. Although many factors may have contributed to this decline, the growth of laparoscopic hysterectomy was a possible contributing factor since the vaginal hysterectomy rate remained stable over the study period. Future studies are needed to evaluate surgical complications and readmission rates in order to more accurately assess the quality of gynecologic surgical care provided by the VA compared with the civilian sector.
Strengths and Limitations
This study has several important strengths. First, the large sample size from VA nationwide databases included information from all VAMC performing hysterectomies. Second, this study included 10 years of data, with the latest data from 2014, allowing for depiction of both long-term and recent trends.