PHI Barriers and Benefits
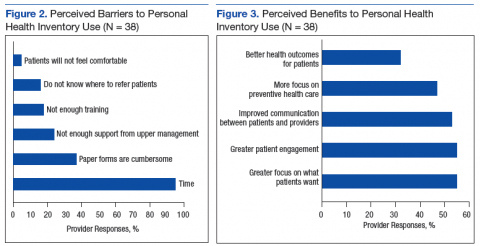
Almost all participants (95%) stated that lack of time was a barrier to using the PHI in their clinical settings (Figure 2). The next most common barriers were cumbersome paper forms (37%) and lack of support from upper management (24%). Very few participants listed discomfort as a reason for not discussing the PHI with patients (5%).
Respondents were divided evenly when identifying the benefits of the PHI. The top 3 selections were greater focus on what patients want (55%), greater patient engagement (55%), and improved patient/provider communication (53%) (Figure 3).
PHI Importance and Future Use
The majority of participants (71%) stated that it was very or somewhat important for VA PCPs to pursue the PHI. However, only 45% planned to use the PHI with their patients. Respondents who said they had implemented the PHI in the past were not more likely than others to state that pursuing the PHI was very important (P = .81). However, respondents who stated that it was very important to pursue the PHI were significantly more likely to plan to implement the PHI (P = .04). Of those planning on its use, the frequency of expected use varied from 31% planning to use the PHI daily with patients to 25% expecting to use it less than once a month.
Discussion
The traditional model of care has been fraught with problems. For example, patients are frequently nonadherent to medical therapies and lifestyle recommendations.3-6 Clearly, changes need to be made. To improve health care outcomes by delivering more patient-centered care, the VA initiated the PHI.7
Although nearly three-fourths of the respondents believed that the PHI was an important tool that the VA should pursue, more than half of all respondents did not intend to use it. Of those planning on using it, a large proportion planned on using it infrequently.
The authors found that despite PCP knowledge of PHI and its acceptance as a tool to focus more on what patients want to accomplish, to enhance patient engagement, and to improve communication between patients and providers, time constraints were a universal barrier to implementation, followed by cumbersome paper forms, and not enough perceived support from local upper management.
Measures to decrease PCP time investment and involvement with paper forms, such as having the patient complete the PHI outside of an office visit with a PCP, either at home, with the assistance of a team member with less training than a PCP, or electronically could help address an identified barrier. Further, if the PHI is to be more broadly adopted, support of local upper management should be enlisted to vociferously advocate its use, thus it will be deemed more essential to enhance care and introduce an organizational system for its effective implementation.
Interestingly, only about one-third of respondents believed that the use of the PHI would lead to better health outcomes for patients. Future studies should address whether the use of the PHI improves surrogate goals, such as cholesterol levels, blood pressures, hemoglobin A1c, or medication adherence as well as harder outcomes, such as risk of cardiovascular outcomes, diabetic complications, and mortality.
Limitations
The questionnaire was used at only 1 health care system within the VA. Whether it could be generalizable to PCPs with other baseline demographic information, non-VA facilities, or even other VA facilities, is not known. Since this survey was administered to PCPs, the authors also do not know the impact of implementing the PHI in specialty settings.
Conclusion
Although the concept of the PHI is favored by the majority of PCPs within VACHS, significant barriers, the most common being time constraints, need to be overcome before it is widely adopted. Implementation of novel collaborative systems of PHI administration may be needed.