Lack of involvement or empowerment. Health care providers often think patients do not act with a sense of empowerment in DM management. Health care providers commonly perceive patients as lacking the motivation to change and say that as many as 30% of patients are uncooperative, regardless of proposed changes .13 Many are convinced that patients are unwilling to make even small lifestyle adjustments, such as getting physically active and losing weight. Health care providers say patients do not ask questions about DM selfmanagement during visits and often do not verbalize how HCPs can best support their needs. 15 They say that patients are so entrenched in their habits, they even refuse DM education. 13
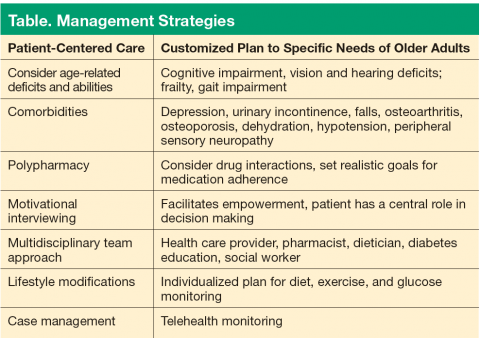
Management Strategies
Several strategies can be deployed to overcome barriers in DM care. Of utmost importance is the need to provide patient-centered care with age-specific characteristics of older adults (Table). To foster mutual collaboration in DM care, HCPs need to ask patients about their health care goals. Patients often view their health through a functional and social perspective rather than from a biomedical perspective. In one study, 71% of patients said their most common health goal was to be independent with activities of daily living, which was more important than the specific details of DM care. 16 Preventing DM complications was among their secondary health care goals.
A DM care plan for older adults should be individualized with careful consideration given to medical history, functional capacity, home care environment, and life expectancy. Many older adults have health problems, such as impaired vision, cognitive impairment, depression, and peripheral sensory neuropathy. They may have osteoarthritis of the knees, osteoporosis of the hip and spine, or urinary incontinence; all these conditions increase the risk for falls. Many older adults are on multiple medications, which can increase falls by causing dizziness, dehydration, or hypotension. 17 Polypharmacy can negatively impact one or more comorbid conditions and QOL. 18
The clinical guidelines for DM management are based on studies conducted in younger populations. However, the 2015 guidelines from the American Diabetes Association (ADA) have been tailored to consider level of health, frailty, cognition, comorbidities, and life expectancy of older adults. The 2015 ADA recommendations provide a framework to guide treatment goals in older adults. A reasonable goal for healthy older adults with few chronic diseases, intact cognition, high functional status, and an anticipated longer remaining life expectancy is an A 1c of < 7.5%. 19 For older adults with comorbidities of intermediate complexity, such as mild cognitive impairment, an A 1c treatment goal of < 8.0% is suggested. An A 1c goal of < 8.5% is recommended for older adults in poor health, such as those with end-stage chronic disease, significant cognitive impairment, or those in long-term care. Health care providers may choose to further individualize A 1c treatment goals to < 7% if patients are healthy and if treatment burdens are not severe or excessive. 19
Multidisciplinary Collaboration
Chronic illness in older adults can be complex to manage due to competing comorbidities and polypharmacy. A diabetes care team consisting of a dietician, social worker, pharmacist, and certified diabetes educator is well suited to effectively manage DM in older adults. Up to 10 hours of DM education with a registered dietician or certified diabetes educator is covered under Medicare in a 12-month period if at least one of the following criteria are met: new diagnosis of DM with A 1c > 8.5%, recent initiation of medication, or a high risk for complications. 20