Across all 13 counties surveyed, rates of underimmunization increased from 8.1% in 2001-2005 to 12.4% in 2010-2012; the peak rate in a single year was 13%, achieved in 2010, while the mean annual increase in underimmunization across all 13 counties was 5.9%. In terms of race/ethnicity, higher percentages of Asian and Hispanic subjects were fully immunized compared with those who were white, black, or of unknown race/ethnicity.
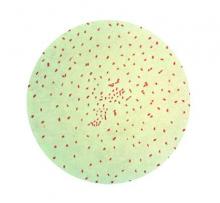
Children in the most statistically significant cluster – the East Bay area, from Richmond to San Leandro – had 1.58 (P < .001) times the rate of underimmunization as displayed by other clusters, with 650 actual underimmunized cases during 2010-2012. Vaccine refusal was also clustered, with rates of 5.5% to 13.5% within clusters, compared with 2.6% outside of them.
Underimmunization of measles, mumps, and rubella and varicella vaccines also clustered in similar geographic areas, a cause for great concern given the recent outbreaks of measles at the Disneyland theme park in Anaheim, Calif. A study published last year, highlights the greater need for health care providers to educate parents about the importance of MMR vaccinations, saying that by doing so, they greatly increase the likelihood of parents agreeing to have their children properly vaccinated (Pediatrics 2014;134:e675-e83). Outbreaks of pertussis also have proved troublesome in recent years, exacerbating the need for greater intervention regarding vaccinating children early and when necessary.
“The existence of clusters may put clinical groups in these locations at a disadvantage in achieving immunization quality benchmarks,” noted Dr. Lieu and her coauthors, adding that “nonmedical exemptions from immunization in California clustered geographically and were associated with clusters of pertussis cases [and] many previous studies have found that vaccine refusal and delay are associated with elevated risk of measles and pertussis outbreaks, as well as elevated individual risks of measles, pertussis, varicella, and pneumococcal infections.”
Funding was provided by a Patient-Centered Outcomes Research Institute Pilot Project contract. Coauthor Dr Klein receives research support from Merck, GlaxoSmithKline, MedImmune, Novartis, Pfizer, Sanofi Pasteur, and Nuron Biotech; no other authors reported any relevant financial disclosures.