Marburg Heart Score and other tests can help rule out ACS
As part of your initial physical examination, assess the patient’s overall condition and stability. Be aware, however, that an older literature review found that a physical exam is only minimally helpful in assessing ACS risk in a patient with chest pain. Findings that may increase the risk of ACS are a third heart sound (positive likelihood ratio [LR+] = 3.2; 95% confidence interval [CI], 1.6-6.5), systolic blood pressure <80 mm/Hg (LR+ = 3.1; 95% CI, 1.8-5.2), and pulmonary crackles on auscultation (LR+ = 2.1; 95% CI, 1.4–3.1); however, the absence of these findings does not exclude ACS.10 The most helpful sign or symptom in evaluating a patient with chest pain is chest wall tenderness on palpation, which largely rules out ACS in low-prevalence settings, such as a primary care office.11
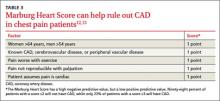
Bösner et al12 developed the Marburg Heart Score (MHS) to help primary care physicians evaluate the risk of CAD in patients with chest pain (TABLE 3).12,13 A subsequent validation study found that an MHS ≥3 had a sensitivity of 89.1% (95% CI, 81.1%-94%) and a specificity of 63.5% (95% CI, 60%-66.9%) for CAD.13 The test’s negative predictive value (NPV) of 97.9% (95% CI, 96.2%-98.9%) means that patients with an MHS ≤2 are very unlikely to have CAD; however, the low positive predictive value (PPV) of only 23.3% (95% CI, 19.2%-28.0%) means an MHS ≥3 is not particularly helpful in diagnosing CAD.12,13
Unless it is clear that your patient’s chest pain is unlikely to have a cardiac cause (eg, pain is reproducible on palpation, or an MHS ≤2), order an electrocardiogram (EKG). If the EKG shows ST-segment elevation in 2 or more contiguous leads, presumed new left bundle branch block, ischemic ST-segment depression >.5 mm (.05 mV), or dynamic T-wave inversion with pain or discomfort, the patient needs urgent referral for emergency care.8 If the EKG is nondiagnostic but the chest pain is suspicious for CAD, then further testing with cardiac biomarkers (eg, troponin I or T) is recommended to evaluate for non-ST elevation myocardial infarction. Consider chest radiography if there is evidence of respiratory disease (cough, dyspnea, or a history of pulmonary disease).
Don’t overlook chest wall syndrome, GERD, or panic disorder
There are several conditions to consider in the differential diagnosis of patients whose chest pain does not appear to have a cardiac cause:
CWS is the most common cause of chest pain in primary care patients.14,15 While there are several specific types of chest wall pain—including musculoskeletal pain, parietal or intercostal pain, Tietze’s syndrome, and costochondral pain—all are manifestations of a musculoskeletal disorder and associated with tenderness of the chest wall. CWS is not life threatening, but one study found high rates of anxiety (54%-93%) among patients with moderate to severe CWS.14,15
Few trials have evaluated treatments for chest wall pain or costochondritis, though typical recommendations include nonsteroidal anti-inflammatory medications, use of heat or cold, physical therapy, or injection of local anesthetic.16 One study found that stretching exercises might benefit patients with costochondritis.17
GI disorders. Patients with esophagitis or gastroesophageal reflux disease (GERD) often report heartburn, chronic cough, chronic laryngitis, and asthma.18 However, the sensitivity and specificity of these symptoms are too low to allow diagnosis or exclusion of GERD based on history alone.18
Acid suppression therapy can be used to test for GERD. A 2005 meta-analysis of 6 studies found the sensitivity and specificity of a proton-pump inhibitor (PPI) acid suppression test for the diagnosis of GERD in patients with noncardiac chest pain were 80% (95% CI, 71%-87%) and 74% (95% CI, 64%-83%), respectively.19 One study demonstrated that relief of chest pain after a 14-day course of omeprazole 40 mg/d was more sensitive than endoscopy, manometry, or 24-hour esophageal pH monitoring in diagnosing GERD.20 Another study found that in patients with noncardiac chest pain and normal upper endoscopy, symptomatic relief with lansoprazole 30 mg/d for 4 weeks can be used to diagnose endoscopy-negative GERD.21
It is appropriate to try a high-dose course of a PPI (ie, omeprazole 40 mg twice daily, lansoprazole 30 mg/d, or esomeprazole 40 mg twice daily) to evaluate for GERD as the cause of chest pain in patients who:20-22
• do not initially describe typical reflux symptoms (eg, heartburn, chronic regurgitation, chronic cough, or a sore or burning throat)
• have no history of surgery in the upper GI tract, esophagus, or thorax, and
• have no signs or symptoms that indicate they have a serious or malignant disease (eg, weight loss, anemia, or dysphagia).