When to introduce insulin
Insulin is indicated for patients with type 2 diabetes whose disease is not easily controlled. That includes individuals with decompensated type 2 diabetes, those whose HbA1c remains high even with 2 or more oral agents, and individuals who have not reached goal after a year of treatment.
Glucose toxicity. It is generally agreed that insulin is the most effective treatment for patients who present with decompensated type 2 diabetes4—ie, with significant hyperglycemia and catabolic symptoms such as polydipsia, polyuria, and weight loss. Initiation of insulin promotes reversal of glucose toxicity and stabilization of metabolic status. In such cases, insulin can be started at a low dose to expose the patient to the complexities of injection therapy (more about this in a bit), then titrated as needed for stabilization.
HbA1c ≥8% even with 2 or more drugs. In my experience, an oral diabetes drug will lead to a drop in HbA1c of about one percentage point. Generally, the further from goal the patient is, the greater the effect the medication will have. As HbA1c inches closer to 7%, the effect diminishes. And when 2 oral agents fail to lower a patient’s HbA1c adequately, the incremental change expected from the addition of a third, fourth, or fifth agent is small.
Thus, in a patient with an HbA1c ≥8%, there is still a significant fasting hyperglycemic component. In such a case, a basal insulin is likely the best treatment option.
Not at goal at one year. Both the AACE and the ADA/EASD guidelines agree that treatment titration should be considered every 2 to 3 months to achieve metabolic control and that if a patient is not at goal after a year, insulin should be started.3,4 However, traditionally this is not done. The delayed implementation of this recommendation is an example of clinical inertia, which can contribute to further misunderstandings about the role and effect of insulin therapy.
Getting started with basal insulin
Most patients who are started on insulin have global hyperglycemia. But because fasting hyperglycemia can affect pancreatic insulin secretion, it is important to get control of the fasting glucose first. This can often be done with insulin sensitizers (metformin, thiazolidinediones, and incretin-based agents).
Suppression of excessive hepatic glucose production, which is very common in type 2 diabetes, is one of the biggest challenges in normalizing fasting glucose. This is well managed with a basal insulin. When starting basal insulin, however, it is critical that current treatments not be stopped. Oral agents such as sulfonylureas and meglitinides can be reduced to lower the risk of hypoglycemia, but stopping them altogether will only prolong the time it takes to get to goal.
There are 3 insulin formulations that can serve as basal insulin (TABLE 1).13 Neutral protamine Hagedorn (NPH) is a human insulin that can be used 2 to 3 times daily to provide basal insulin coverage. But long-acting basal analog insulins glargine and detemir, typically administered once a day when used by patients with type 2 diabetes, are a better option.14
While all 3 formulations have similar efficacy for lowering HbA1c, the analog basal insulins have numerous advantages: less weight gain, less hypoglycemia for the same level of glucose control, and less frequent dosing. In addition, glargine and detemir are available in a pen or vial, while generic NPH is available only in a vial. The primary disadvantage of the analogs is cost: A month’s supply—one vial—of NPH sells for approximately $25 (generic) or $94 (brand name); in comparison, a month’s supply (one box of 5 3-mL pens) of detemir and glargine costs about $300 and $320, respectively.15 (Humulin N, a brand-name NPH, is available in a pen, at a cost of approximately $315 per box.)
Use a weight-based initial dose
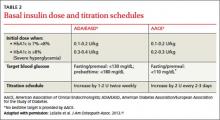
The recommended starting dose is 0.1 to 0.2 U/kg daily for patients with an HbA1c <8%. If HbA1c is ≥8%, the ADA/EASD guidelines recommend a starting dose of 0.3 to 0.4 U/kg daily4(TABLE 2).3,4,16 While basal insulin is most commonly dosed at bedtime, in fact, basal analog insulins can be given at any time that’s convenient for the patient. Morning dosing may be preferable for individuals with a significant fear of hypoglycemia—a phobia that sometimes causes patients to skip insulin doses and engage in “defensive eating” (ie, eating in an attempt to prevent hypoglycemia rather than because of hunger or the need for nutrition).
Teach injection technique