We reported descriptive statistics for categorical and continuous data, and performed between-group statistical comparisons on survey items via the Chi-square test or Fisher’s Exact test when necessary. We performed age comparisons with the Independent t-test. We considered a 2-tailed value of .05 as statistically significant in all analyses, which we conducted with SPSS software (International Business Machines, Chicago, Ill).
RESULTS
All 333 patients invited to participate gave informed consent and completed the survey in its entirety. Patients were evenly distributed by gender. The median age of all patients was 44±13.1 years (range, 19-83). Approximately two-thirds of patients (66%) perceived that discussions with their PC physicians regarding lifestyle modifications and risk factors affecting GERD were “in-depth.”
We examined the gender and age of patients as functions of perceived discussion level. Men and women were equally likely to have in-depth discussions with their physicians (P>.05). On the other hand, younger patients were more likely than older ones to have in-depth discussions. The mean age of the patients who reported having an in-depth discussion was 42.6±13.1 years; of those who did not have an in-depth discussion, the mean age was 46.0±12.9 years (P<.05). However, for each individual survey question, the number of correct responses did not correlate with age, suggesting that age is not a true predictor of level of discussion.
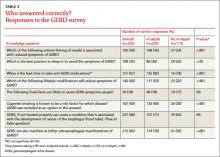
Approximately one-third of patients (32%) were not aware that untreated GERD can be associated with increased risk of cancer of the esophagus, although there was no significant difference between discussion level groups (P>.05) (TABLE 2). Similar numbers of patients reported being aware of best sleeping position (33%), with those in the in-depth discussion group exhibiting a better understanding of the best position (36% vs 26%, respectively; P<.05). Patients perceiving they had an in-depth discussion with their PC physicians were significantly more likely than those in the other group to know the appropriate time to eat dinner (76% vs 24%, respectively; P<.001). Overall and without respect to discussion level, few patients understood dietary guidelines (18%, P>.05).
Patients having an in-depth discussion with their primary care physician were also more likely to know the best time to take antireflux medications (85% vs 18%, respectively, P<.001); that GERD symptoms can be reduced through lifestyle modifications (53% vs 22%, respectively; P<.001); and that GERD can manifest as chronic cough, hoarse voice, or sore throat (79% vs 36%, respectively; P<.001).
DISCUSSION
We conducted a simple, easy-to-use survey to gain an appreciation of patients’ levels of understanding of GERD after discussion with their physicians. Specifically, the survey related a patient’s perceived level of discussion to his or her knowledge of facts pertinent to GERD, including personal lifestyle choices. Importantly, the patient’s perception of the quality of discussion was surveyed, as perception and reality are not always in agreement.
Although the American Gastroenterological Association advocates that physicians should have in-depth discussions with their patients with respect to the disease process and lifestyle modifications, this is not typical.4,7
In our study, 66% of patients perceived that they had an in-depth discussion with their PC physician regarding factors affecting GERD. Of patients taking a PPI, 85% of those having in-depth discussions were aware of the correct time to take their medication. Of those not having an in-depth discussion, only 18% gave the correct answer, which is no better than a random guess (20%) and suggests that, essentially, none of these patients knew when to take their medication.
Study limitations. We did not validate our survey against other surveys or within our patient population; additional efforts are therefore warranted in this regard. Future studies might also explore how duration and severity of symptoms prior to patient-physician discussions, socioeconomic status, and education level influence the relationship between perception of care and understanding of GERD. A follow-up survey would help to define whether these discussions translate into improved disease management.
In spite of the limitations of our survey, our data clearly demonstrate that knowledge of GERD correlates with the perceived level of discussion that patients have with their physician, and that a large percentage of patients do not fully understand their condition and methods to manage it. Patients who did have an in-depth discussion with their primary care provider were likely to be better educated with regard to GERD. Because of the prevalence of GERD,1,7,8 its association with increased health care costs and reduced quality of life,1,8 and predominant management at the primary care level, we recommend that PC physicians place more emphasis on the education of patients diagnosed with GERD.
CORRESPONDENCE
Naser M. Khan, MD, Advanced Gastroenterology Associates, Doctors Office Building 3, Suite 2300b, 1555 Barrington Road, Hoffman Estates, IL 60169; drkhan99@hotmail.com