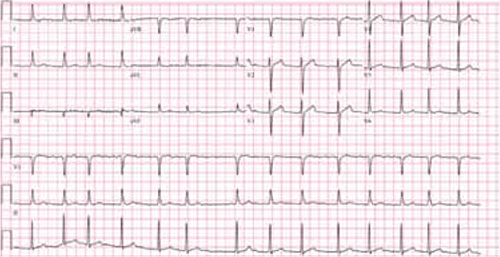
Multifocal atrial tachycardia (FIGURE 3) is a supraventricular arrhythmia with ≥3 different P wave morphologies, as well as varying PR and RR intervals on the 12-lead EKG. It is typically associated with lung disorders but may occur in patients with other conditions, such as theophylline toxicity.14
FIGURE 3
Multifocal atrial tachycardia

The P waves have varied morphologies; the PR and RR intervals also vary, which is best seen in lead V1.
Atrioventricular nodal reentrant tachycardia (AVNRT), a reentrant form of narrow QRS complex tachycardia, is based on a dual (slow and fast) pathway of the compact AV node (FIGURE 4). In the typical form—constituting 90% of cases15—antegrade conduction is via the slow pathway and retrograde conduction is via the fast pathway.16 In the atypical form, it’s the other way around.
FIGURE 4
Atrioventricular nodal reentrant tachycardia

Note the “pseudo S” waves, which is best seen in leads II, III, and aVF. This represents retrograde activation of the atria with an inferior-to-superior axis. The RP interval is very short.
Orthodromic atrioventricular reciprocating tachycardia (AVRT), or Wolff-Parkinson-White syndrome, is a narrow QRS complex tachycardia in which antegrade conduction is via the AV node and retrograde conduction is via an accessory pathway (bundle of Kent). The accessory pathway consists of a band of muscle tissue that connects the atrium directly to the ventricles, allowing electrical impulses to bypass the AV node. Antidromic AVRT, a wide QRS complex tachycardia, is the most common supraventricular arrhythmia in patients with accessory pathways.17
Atrial fibrillation (FIGURE 5), the most common arrhythmia for which medical treatment is required,18 is an irregular rhythm with an undulating baseline.19
FIGURE 5
Atrial fibrillation
This strip shows an irregularly irregular rhythm with no distinct P waves. The undulating baseline represents fibrillatory waves.
Atrial flutter is a reentrant tachycardia originating in either atrium, with regular flutter (F) waves on a 12-lead EKG (FIGURE 6). A counterclockwise propagating isthmus-dependent atrial flutter originating in the right atrium produces the typical “sawtooth” pattern of negative F waves in the inferior electrocardiographic leads.
FIGURE 6
Atrial flutter

Note the regular flutter waves (“sawtooth waves”) best seen in lead II with variable AV conduction.
Junctional ectopic tachycardia is a rare arrhythmia caused by increased automaticity within the bundle of His.20,21 It is typically diagnosed in childhood and usually presents as a narrow QRS tachycardia with AV dissociation,22 but retrograde conduction to the atrium has also been found.21
How to approach the differential diagnosis
There are a number of characteristics to consider in the differential diagnosis of a patient with narrow QRS complex tachycardia (ALGORITHM).1,23-29 These include:
- rhythm regularity
- P wave axis and morphology
- relative duration of RP and PR intervals
- P wave position relative to the QRS complex
- ST elevation in lead aVR
- onset and termination mode.
ALGORITHM
Narrow QRS complex tachycardia: Zeroing in on the diagnosis1,23-29

AVNRT, atrioventricular nodal reentrant tachycardia; AVRT, atrioventricular reciprocating tachycardia; EKG, electrocardiogram; MAT, multifocal atrial tachycardia.
*Or technically poor EKG.
Rhythm regularity is a key consideration. An irregular rhythm and the absence of P waves (or the presence of fibrillatory waves) characterizes atrial fibrillation; irregularity and ≥3 different P wave morphologies is suggestive of multifocal atrial tachycardia. Other possibilities include frequent premature atrial contractions or a sinoatrial or AV nodal conduction block.
AV dissociation is rarely seen in narrow QRS complex tachycardia. Its presence raises the possibility of junctional ectopic tachycardia, ventricular tachycardia, or complete AV node block.
P wave axis and morphology can help with both the differentiation and the origin of narrow QRS complex tachycardias. A superior-to-inferior axis of P waves (positivity in leads II, III, and aVF) is seen in sinus node-generated tachycardias and sometimes in focal atrial tachycardia. An inferior-superior P wave axis (negativity in leads II, III, and aVF) is observed in AVNRT, AVRT, and a subset of focal atrial tachycardia.23,24
The specific P wave axis and morphology in focal atrial tachycardia depends on the site of atrial automaticity. If the origin is near the sinus node region or high in the atrium, the result would be a superior-to-inferior P wave axis; if it originates lower in the atrium, the resulting atrial depolarization would be an inferior-to-superior axis.23,24
Relative duration of RP and PR intervals can help to differentiate narrow QRS complex tachycardias based on the timing of the P wave with respect to adjacent QRS complexes. Those in which the RP interval is longer than the PR interval are called long RP tachycardias and include sinus tachycardia, intra-atrial tachycardia, atypical AVNRT, and AVRT with a slowly conducting ventriculoatrial pathway.25,26

