• Order blood cultures for febrile patients who are suspected IV drug users. Doing so is wise because of the high morbidity and mortality associated with infectious endocarditis.
• Consider the possibility of a false-positive monospot test in patients who have leukemia, lymphoma, pancreatic cancer, systemic lupus erythematosus, HIV infection, or rubella.
CASE A 27-year-old man came into our emergency department (ED) with a 1½ week history of profound nausea, vomiting, diarrhea, intermittent fevers, and weight loss of 15 pounds. At the urging of his mother, he had recently visited a new family physician to investigate a 3- to 4-month history of fatigue and anorexia. According to the patient, the blood work done by the FP was normal, but since that visit things had gotten worse.
The patient denied any ill contacts or recent travel. He said he had no headache, neck stiffness, sore throat, cough, dysuria, back pain, rash, focal numbness, or weakness. His past medical history was significant for prescription drug abuse, and he was now on buprenorphine and naloxone (Suboxone) treatment. He initially denied IV drug use, but later acknowledged it after the discovery of syringes and heroin among his personal belongings.
On physical exam he appeared cachectic and tremulous. His temperature was 101.4°F; heart rate 139 beats per minute, blood pressure 83/43 mm Hg, and SpO2 93%. His pupils were small, conjunctiva pale, and sclera white. His oropharynx was without lesions. The rest of his physical exam was unremarkable.
Laboratory results in the ED revealed a white blood cell count of 14,600 cells/mcL, platelets 85,000/mcL, hemoglobin 11.8 g/dL, and creatinine 2.04 mg/dL. He had a positive monospot test. We sent out blood and urine cultures, as well as human immunodeficiency virus (HIV) and Epstein-Barr virus (EBV) serologies. Imaging included a chest x-ray, which showed possible nonsegmental or mild perihilar airspace disease.
The patient was admitted to the hospital for sepsis with associated acute kidney injury, dehydration, and weight loss.
Although the patient had a positive monospot test, the severity of the clinical picture did not fully match that of infectious mononucleosis. Also, it seemed curious to us that a high-risk patient would contract EBV for the first time at age 27.
Given the patient’s clinical presentation and the fact that he was an IV drug user, we suspected HIV infection. But an HIV-1 RNA quantitative PCR test came back negative.
What is the Most Likely Explanation for his Condition?
Infectious endocarditis
Our patient was admitted to the telemetry unit, given aggressive IV hydration, and started empirically on vancomycin secondary to the risk for infectious endocarditis (IE). On hospital Day 1, the patient’s blood cultures returned positive for methicillin-sensitive Staphylococcus aureus and an echocardiogram revealed a large tricuspid vegetation (FIGURE 1).
IE is relatively common in IV drug users, affecting up to 2% to 5% of this population each year in the United States.1 Onset of symptoms is usually acute, and in many cases, there is no heart murmur or peripheral stigmata of IE.1
Blood cultures are positive in 69% to 97% of cases of IE,2 with more than 50% caused by S aureus.3 The most common valve infected is the tricuspid valve (30%-70%), especially when related to IV drug use.1 More than half of IV drug users with tricuspid IE will have extracardiac infections, most often occurring in the lungs, bone, kidneys, and brain.3
Because of the high morbidity and mortality associated with IE, physicians caring for febrile patients who are suspected IV drug users should order blood cultures. Three blood draws should be taken, at 30-minute intervals, from separate venipuncture sites.4 Positive cultures should be followed by an echocardiogram to rule out IE. For severely ill patients, empiric antibiotics should be started.4
FIGURE 1
Echocardiogram reveals tricuspid vegetation
Treatment is complicated for IV drug users
Treatment for IE is with IV antibiotics. This can be complicated in the case of an IV drug user, as he or she may be unwilling to remain hospitalized for the duration of treatment. In addition, there are ethical concerns about sending such patients into the community with an indwelling IV.
Cardiac surgery is a possibility. Complications of IE that warrant surgery include repeated septic emboli with large vegetation, heart failure secondary to aortic or mitral-valve regurgitation, persistent fever after 8 days of appropriate antibiotic therapy, infection with certain difficult-to-cure microorganisms, and perivalvular abscess development.5
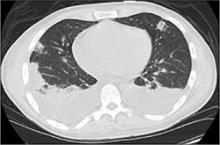
FIGURE 2
Chest CT shows pulmonary emboli
Successful valve repair for our patient
Our patient’s hospital course was complicated by the development of pulmonary septic emboli (FIGURE 2) and persistent fever. He underwent a successful tricuspid valve repair and was discharged with a peripheral IV to a skilled nursing facility to complete a 6-week course of IV cefazolin.