Consensus guidelines weigh in on SCD risk
Age is another consideration in risk stratification for SCD, which primarily strikes those with HCM in adolescence or early adulthood. Consensus guidelines from the American College of Cardiology (ACC), American Heart Association (AHA), and European Society of Cardiology (ESC)21 (TABLE 1) offer additional considerations in assessing SCD risk.
Risk factors identified as “major” in the consensus guidelines include unexplained syncope, family history of premature cardiac death, left ventricular wall thickness ≥30 mm, abnormal blood pressure response to exercise, and nonsustained ventricular tachycardia, as well as a prior episode of cardiac arrest—the single most predictive risk factor.22 Because of the high risk of sudden death, exercise is absolutely contraindicated for many patients with certain HCM phenotypes and major risks.
The organizations also cite “possible” risk factors, and indicate in consensus statements that patients with more than 1 major or other possible risk factors are at higher risk for SCD.6,21 In cohort studies, however, other than a prior episode of cardiac arrest, no other risk factor has been found to predict SCD.
Cardiac MRI, discussed earlier for diagnostic purposes, may also have a role in stratifying risk. In small studies conducted recently, the presence of myocardial fibrosis (as demonstrated by delayed gadolinium enhancement) correlates with increased risk of nonsustained ventricular tachycardia (RR, 1.6, compared with HCM patients without myocardial fibrosis).23
HCM management: Pharmacologic and surgical options
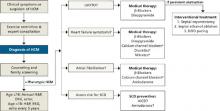
There are no large-scale studies of medical treatments for HCM, and therapy is largely empiric and individualized based on complications, symptoms, and risk (FIGURE).24
FIGURE
HCM: A guide to screening, diagnosis, and treatment
*Relatively contraindicated in LVOTO patients.
AICD, automatic implantable cardioverter defibrillator; DDD, dual-chamber; echo, echocardiography; EKG, electrocardiography; HCM, hypertrophic cardiomyopathy; H&P, history and physical; LVOTO, left ventricular outflow tract obstruction; SCD, sudden cardiac death.
Adapted from: Soor GS, et al. J Clin Pathol.4
Which drugs for which patients?
For those with symptoms of heart failure, beta-blockers are first-line therapy. Additional therapeutic options for patients without LVOTO include calcium channel blockers, nitrates, and diuretics. But these additional therapies are relatively contraindicated in patients with LVOTO. For LVOTO patients, disopyramide can be added to the beta-blocker regimen, if needed for symptom control.4,24
Patients with LVOTO or abnormal mitral motion are at moderate risk of spontaneous bacterial endocarditis (SBE).18 But evolving evidence shows low baseline rates of SBE and increased complications in patients routinely receiving antimicrobial prophylaxis, so the most recent guidelines do not recommend such treatment for any HCM patient.25
Amiodarone is effective for atrial fibrillation in HCM when beta- or calcium channel blockers fail to provide sufficient rate control.4 Amiodarone can also be used to prevent SCD.26 Recent data show that an automatic implantable cardioverter defibrillator (AICD)—which we’ll discuss later—is superior to amiodarone in preventing SCD,27 but the drug may be used in addition to an AICD or given to patients who are not candidates for, or not interested in, an implantable device.22,24
Invasive treatments may be considered for patients with LVOTO who do not respond to medical management.
Septal myomectomy or ethanol ablation: Which is better?
Septal myomectomy is the gold standard for refractory LVOTO.28 This open-heart procedure, which involves the resection of a portion of the septum to remove the obstructing cardiac tissue, has an operative mortality rate <1%.28 Surgical complication rates are also low, but include aortic regurgitation, left bundle or complete heart block, and iatrogenic ventricular septal defect.
Septal ethanol ablation is a percutaneous alternative to surgical myomectomy. In this minimally invasive procedure, ethanol is injected into the first septal perforating branch of the left anterior descending (LAD) artery, resulting in myocardial necrosis and septal wall thinning, which relieves the obstruction. Complications include ablation of inappropriate myocardium, heart block, pericardial effusion, and LAD dissection.29 Maximum effects of the ablation are delayed, typically occurring 6 to 12 months after the procedure.
Although limited by a lack of randomized controlled trials, a recent meta-analysis found surgical myomectomy and ethanol ablation to be equally effective in decreasing the LV outflow gradient to <20 mm Hg. Notably, though, surgical myomectomy reduced the gradient to nearly 10 mm Hg, compared with an average of 18 mm Hg for ethanol ablation.28 What’s more, several studies have found a higher incidence of complete heart block in patients who had ethanol ablation compared with those who underwent myomectomy.30 For patients who cannot tolerate or are not interested in invasive surgery, ablation offers an effective option.
Dual-chamber (DDD) pacing can also be used to treat LVOTO, but studies comparing pacing with myomectomy and ablation have found mixed results.6 Despite recent data showing the benefits of pacing in HCM,31 DDD pacing is typically reserved for patients who are not candidates for either surgical myomectomy or ablation.4