The physician-owners of everyday Primary Care, feeling stressed out and recognizing that “things are not good here,” signed up to participate in 1 of our studies. Participation required allowing an outside facilitator to observe practice operations and conduct open-ended interviews with physicians and staff over a 2-week period, followed by a series of 12 weekly meetings. In addition, physicians and staff agreed to fill out multiple surveys during the study process and allow researchers to audit the charts of randomly selected patient samples.
One year after Everyday Primary Care signed up, the office space was still cramped, the financial situation was no better, and environmental pressures were continuing to mount. And yet, the practice felt like a different place, one filled with energy and hope. What had happened?
RAP, huddles, effective teams. Most importantly, the quality and types of relationships within the practice had changed. At our suggestion, the practice formed a RAP (reflective adaptive process) team under the guidance of a facilitator—a nurse we trained in basic facilitation skills, including effective meeting strategies, brainstorming, and conflict resolution. The team consisted of physician leaders (both Drs. Cope and Varimore attended all meetings), the practice manager, representatives from each part of the practice (billing, front desk, nursing staff, insurance clerk), and a patient.15 The RAP intervention was designed to provide members with time and space to reflect and opportunities to learn the value of communication, respectful interaction, and listening to diverse opinions and perspectives.20 The team met with the facilitator for 1 hour every week, reviewed the practice’s vision, and developed and implemented strategies for solving prioritized practice issues and problems.
Brainstorming helped identify recurrent problems. As the RAP meetings progressed, it became clear that despite the close quarters, each part of the practice was isolated from the others and all team members were frustrated by their inability to influence the lead physician, Dr. Cope. Over time, the RAP meetings changed the relationship patterns and the quality of communication, thus helping the practice move forward and get unstuck. Dr. Cope repeatedly commented, “I didn’t know that,” as staff shared their concerns and challenges. For example, Dr. Cope was amazed when the front desk described the amount of time and degree of disruption caused by drug reps constantly coming into the office. Together, the team was able to come up with a solution—setting aside a special time for drug reps, rather than allowing them to arrive whenever they chose—that worked for physicians and staff alike.
Our current project notes from Everyday Primary Care reflect a very different and vibrant practice, in which the atmosphere is charged with hope and everyone reports being more relaxed—though just as busy. Office processes have improved and space is less cluttered. Chart audit scores reveal improved quality of chronic care and preventive services. Because practice members have learned to communicate across the barriers of job classification and hierarchy, they are able to solve problems as they arise without allowing things to fester. These improved relationships led to an enhanced understanding of complex issues like patient triage and scheduling and more numerous and accurate memories of how the practice has operated over the years.21-23
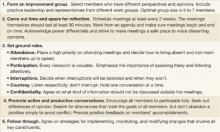
Our research has taught us that practices that pay attention to building strong relationships are better able to deal with the surprise and uncertainty that characterize modern health care delivery.24-26 The primary care management literature has highlighted a number of practical strategies for enhancing relationships and communication, including the use of RAP teams, huddles, effective team meetings, and high-performing clinical teams.15,27-29 In addition, we refer the reader to The Team Handbook, 3rd ed., by Peter R. Scholtes, Brian L. Joiner, and Barbara J. Streibel. The handbook contains a wide range of practical teambuilding strategies in an easily accessible style.30 FIGURE 1 summarizes 5 tips for building critical relationships in your own practice.
FIGURE 1
5 tips for building critical relationships
Interact with the “local fitness landscape”
Our second insight is that practices must learn to interact with what we call the “local fitness landscape.”31-33 To understand what that term implies, imagine your hometown with multiple primary care offices of different sizes, a variety of specialty practices, 2 or 3 competing hospital systems, multiple insurance options, businesses, housing clusters representing different social classes, schools, banks, scattered farms, industries, waterways, animals and plants, transportation systems, and political and religious institutions. The totality of all these elements is the local fitness landscape.